Skin Picking OCD (Dermatillomania) Treatment
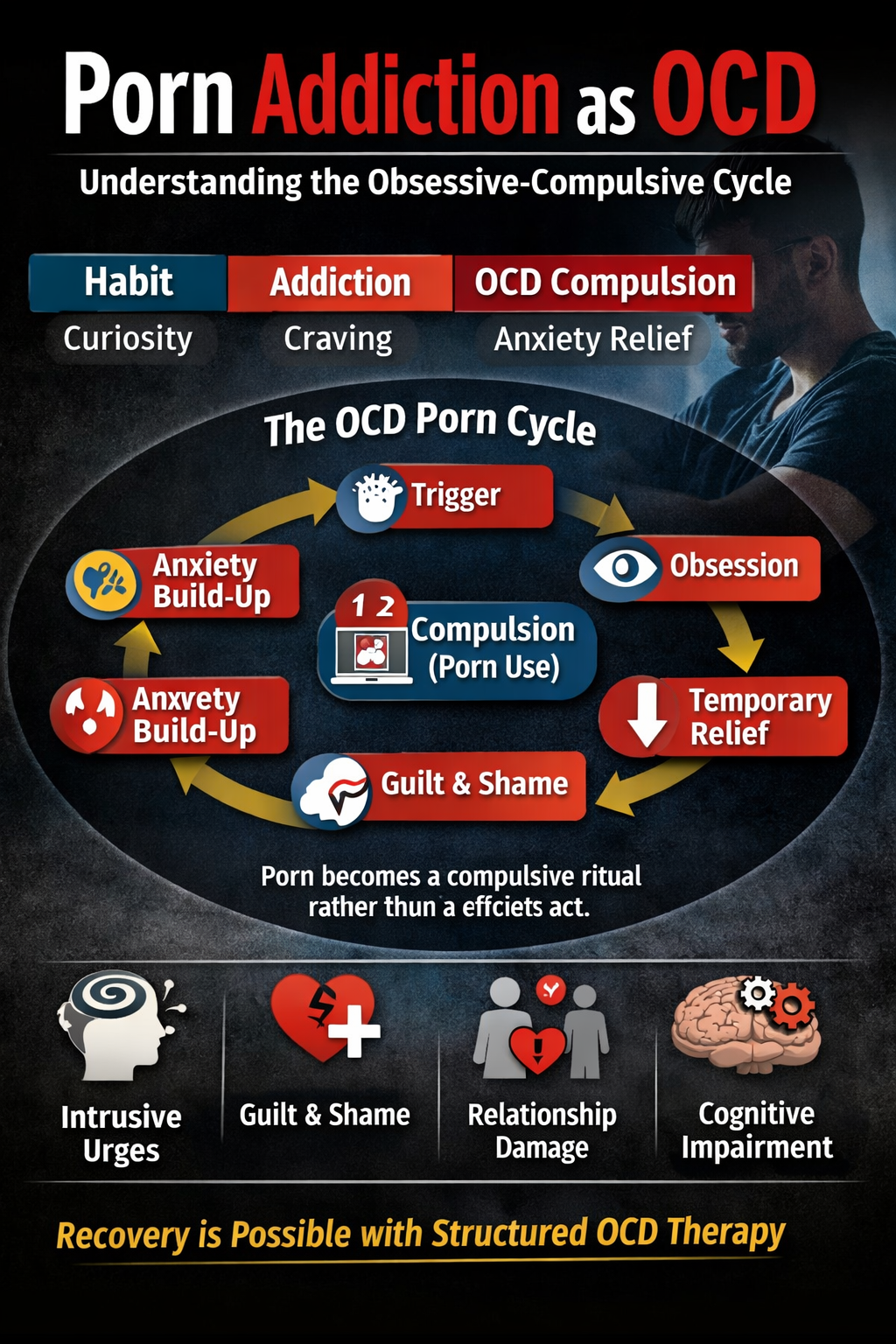
Skin Picking OCD is also known as Dermatillomania OCD is a rare form of OCD subtype but when it is present it is extremely distressing for a person who is dealing with it. The act of picking at one’s skin may seem like a harmless habit for some, but for others, it’s a compulsive behaviour that can lead to significant physical and psychological distress. Known as Dermatillomania or Excoriation Disorder, skin picking is more than just a fleeting impulse for many. Skin Picking OCD, clinically known as Excoriation Disorder or Dermatillomania, is a Type of OCD characterized by repeated and compulsive picking of the skin, leading to skin lesions. This behaviour may be a way of dealing with negative emotions or stress. While many people might pick at their skin from time to time, those with Dermatillomania do it habitually, often without realizing & find it challenging to stop, even if they want to.
Causes of Skin Picking OCD / Dermatillomania and OCD
Combination of factors is believed to contribute in development of Skin Picking OCD:
- A. Family history of Obsessive Compulsive Disorder (OCD) might increase the likelihood of Skin Picking OCD.
- B. Many individuals pick their skin as a way to cope with anxiety, stress, or other emotions in Skin Picking OCD.
- C. Sensory Stimulation: Some people find the act of skin picking to be satisfying or pleasurable.
Impact of Skin Picking OCD in Life
While the physical effects, such as scars or infections, are visible, the emotional toll can be even more profound:
- A. Isolation: Due to feelings of embarrassment or shame, many hide their condition in Skin Picking OCD.
- B. Decreased Self-Esteem: Visible marks and scars can lead to self-consciousness and a decline in self-worth in Skin Picking OCD.
- C. Anxiety & Depression: Continual skin picking and the consequences thereof can exacerbate feelings of anxiety and depression is common in Skin Picking OCD.
Symptoms of Skin Picking OCD or Dermatillomania
- Regularly picking at skin, often to the point of causing damage or scars.
- Repeated attempts to stop or decrease skin picking.
- Picking in response to feelings of anxiety, boredom, or tension.
- Feeling a sense of relief or satisfaction after skin picking.
- Hiding or being embarrassed about the skin-picking behaviour.
- Having noticeable skin damage, such as scars, open sores, or discoloration.
- Spending a significant amount of time picking at the skin or dealing with its consequences.
- Interference with daily life due to skin picking (Avoiding social situations and social interaction).
Treatment for Skin Picking OCD and Skin Picking Without Medicine (Natural Treatment)
Skin picking OCD might seem as a mere skin allergy which they would often not consider significant but to those who experience it as a compulsion it takes a major toll on different areas of their lives and most of the times such people aren’t fully aware of what triggers lead to skin picking in them. Before it gets worse, people who have Skin Picking OCD as a compulsion must reach out to a Psychotherapist in order to receive the best treatment possible.
Some of the major psychotherapies/ psychological approaches that have been result oriented/ have given the best results for skin picking are:
Cognitive Behavioural Therapy (CBT)
CBT can help individuals recognize the triggers for their skin-picking behaviour and develop healthier coping mechanisms. A specific form of CBT called Habit Reversal Training (HRT) has been particularly effective for it. HRT helps individuals become more aware of their picking and the situations in which they pick, and then teaches them to engage in a competing response when they feel the urge to pick.
Acceptance and Commitment Therapy (ACT)
This form of therapy can help individuals accept their urges without acting on them and commit to making behavioural changes based on personal values.
Mindfulness and Meditation
Focusing on the present and developing greater self-awareness can help individuals resist the urge to pick and recognize when they’re doing it.
Exposure and Response Prevention (ERP)
This is a technique derived from CBT and used primarily for OCD. It exposes individuals to the situation that triggers their urge to pick but prevents them from engaging in the picking behaviour.
Dialectical Behaviour Therapy (DBT)
Originally developed for individuals with borderline personality disorder, DBT can also help those with skin picking. It teaches coping skills to deal with stress and regulate emotions, which can reduce the urge to pick.
Conclusion
In conclusion, Skin picking is a challenging condition, but with awareness, support, and appropriate intervention, many individuals can reduce or manage their skin-picking behaviors and improve their overall well-being.
A Case Study on Skin Picking OCD
Reshu, 27 Years
Background
Reshu is a 27-year-old software engineer who works at a reputable technology company. She’s lived in a city apartment for five years, is single, and has a close group of friends. Despite her achievements, Emily has been dealing with an uncontrollable urge to pick at her skin for the past 10 years.
Presenting Problem
Emily seeks therapy due to increasing distress over her skin-picking habits. She has noticeable scabs and scars on her arms, legs, and face. She confides that her picking sessions can last anywhere from minutes to hours, especially during high-stress periods.
History
Emily first remembers picking her skin during her teenage years, particularly during exam times. Initially, it was an unconscious act, but over the years, it has become a way for her to cope with stress, anxiety, and boredom.
Impact on Daily Life
- Social Impact: Emily avoids social situations where her skin would be exposed, like pool parties or beach outings. She has started wearing long sleeves and pants even in hot weather to cover up the scars.
- Professional Impact: She finds herself picking during virtual meetings when her video is off. Emily sometimes takes longer to complete tasks because she gets lost in a picking session during work hours.
- Emotional Impact: Emily feels a mix of relief and intense guilt after picking. She’s increasingly self-conscious about her appearance and fears judgment from others.
Assessment and Diagnosis
After thorough assessment, the therapist diagnoses Emily with Skin Picking Disorder (Dermatillomania), a type of OCD.
Treatment Plan for Finger Skin Picking OCD
- Cognitive Behavioural Therapy (CBT): Emily starts attending weekly CBT sessions. Here, she learns to identify triggers that cause her to pick, such as feelings of anxiety or the texture of a scab. She’s introduced to healthier coping mechanisms like deep breathing exercises or using a fidget toy.
- Habit Reversal Training (HRT): This involves becoming more aware of the habit and replacing the skin-picking behaviour with another action, such as clenching her fists or playing with a stress ball.
- Skin Care: A dermatologist helps Emily with a skincare routine to heal her skin and reduce the temptation to pick at imperfections.
Frequently Asked Questions (FAQ) – Skin Picking OCD
1. What is Skin Picking OCD (Excoriation Disorder)?
Skin Picking OCD, also called Excoriation Disorder or Dermatillomania, is a mental health condition where a person feels strong urges to pick at their skin, often leading to wounds, scabs, or scars. It is considered part of the OCD and related disorders spectrum.
2. Is skin picking the same as a bad habit?
No, it is not just a habit. While some people may occasionally pick at their skin, Skin Picking OCD is driven by obsessive urges and compulsions. It can cause significant distress, damage to the skin, and difficulty in daily life.
3. What causes Skin Picking OCD?
The exact cause is not fully known. It may be linked to anxiety, OCD, perfectionism, or an attempt to cope with stress.
4. Can Skin Picking OCD be treated?
Yes. Effective treatments include Cognitive Behavioral Therapy (CBT), especially Habit Reversal Training (HRT) and Exposure and Response Prevention (ERP). In some cases, medication may also be prescribed by mental health professionals.
5. How do I know if I or my loved one has Skin Picking OCD?
If the skin picking is repetitive, hard to control, leads to skin damage, causes shame or anxiety, and interferes with daily life, it may be a sign of Skin Picking OCD. A professional diagnosis from a trained therapist or psychiatrist is recommended.
6. Can Skin Picking OCD cause health problems?
Yes, frequent picking can lead to infections, scarring, and skin damage. It can also impact emotional well-being, leading to guilt, low self-esteem, or social withdrawal.
7. How can family members support someone with Skin Picking OCD?
Avoid criticism, be patient, and encourage professional help. Offering emotional support, creating a calm environment, and learning about OCD can make recovery smoother.
8. Can mindfulness or self-help techniques reduce skin picking urges?
Yes, strategies like mindfulness, stress management, using fidget tools, or covering vulnerable areas can help reduce urges. However, professional therapy provides long-term results.
Contact Emotion of Life
Call now: +91 9368503416
Website: www.emotionoflife.in
Email: info@emotionoflife.in
Book Now | OCD Types | Meet Our Experts | Success Stories | Contact Us