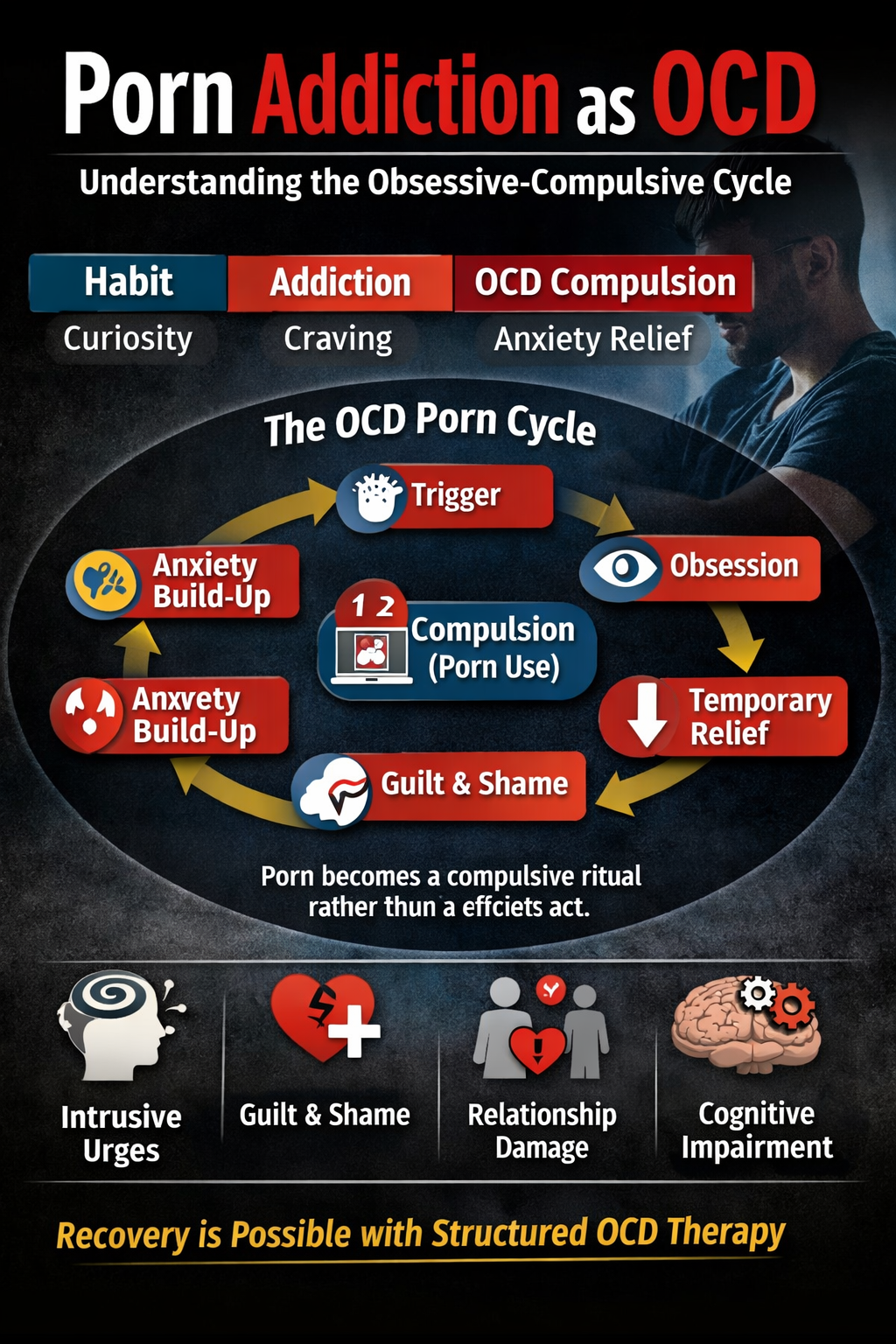
OCD of rumination is a distressing type of OCD where individuals become trapped in prolonged, repetitive thoughts that seem impossible to stop. These ruminative thoughts are intrusive and conflict with one’s sense of self, focusing on “what if” scenarios, moral uncertainties, reflections on past experiences, existential queries, or hypothetical disasters, rather than facilitating problem-solving. Similar to other OCD types, OCD of rumination creates a feedback loop where intrusive thoughts trigger significant anxiety, leading the person to engage in mental rituals that provide temporary relief but reinforce the cycle. Terms like OCD of rumination, OCD of rumination, obsessive rumination, and mental compulsions are crucial for understanding this disorder, as they describe both the symptoms and the mechanisms that sustain it.
OCD of rumination is often referred to by various names such as OCD of rumination, cognitive OCD, or reflective OCD but they all share the trait of prolonged mental examination without the presence of overt physical rituals. Focus areas for ruminations include feelings of moral guilt, doubts about relationships, questions about existence, or fears of having harmed others, often misleadingly perceived as merely “thinking things through.” The distinction lies in the nature of the reflection: while healthy contemplation leads to conclusions and choices, OCD of rumination is marked by repetitive, distressing, and paralyzing cycles. Since the topics often involve considerations that anyone might ponder like ethics, identity, or memories, individuals may feel embarrassed or invalidated, questioning why regular contemplation has turned into a mental prison.
Types of OCD of rumination
OCD of rumination manifests in various ways.
- Some individuals become trapped in moral reflections, continually replaying interactions and worrying about having behaved unkindly without evidence.
- Others may experience existential ruminations, where they obsess over the nature of reality or life’s meaning, hindering their ability to make decisions.
- Relationship ruminations are also common, with individuals rethinking conversations or constantly analyzing their partners’ words and actions.
- Health-related ruminations can manifest as excessive monitoring for signs of illness. The resulting mental rituals, although subtle, can be powerful such as counting thoughts or mentally arguing against them serving to temporarily relieve anxiety and reinforcing the compulsive behavior for future intrusive thoughts.
Impacts of OCD of rumination
The influence of OCD of rumination on daily life is frequently underestimated.
- Time is consumed by mental loops, diminishing availability for work, relationships, and enjoyment.
- Decision-making becomes arduous, as every choice is dissected to an extreme like should I take the job? Did I offend my friend? Do I truly want this? Sleep is often disrupted, leading to chronic fatigue and irritability, along with a pervasive sense of being “stuck.”
- Socially, the disorder can weaken intimacy since partners and friends may become sources of repeated reassurance, perpetuating the compulsive behavior.
- Emotionally, shame and self-doubt escalate as individuals question the purpose and relentlessness of their thoughts.
Causes of OCD of rumination
The causes of OCD of rumination are varied.
- Personality traits: play a role, as those who are reflective, perfectionistic, or intolerant of uncertainty may misinterpret fleeting thoughts as important issues that demand resolution.
- Life events: such as relational stress, moral dilemmas, traumatic experiences, or significant transitions often serve as catalysts for rumination.
- Cultural and familial influences: which may encourage constant introspection, increase doubt with moral failure, or impose punitive views of uncertainty can also trigger individuals for rumination. Furthermore, modern elements like the constant availability of information and social comparison can heighten cognitive overload, providing more material for rumination.
Treatment for OCD of rumination
Effective treatment for OCD of rumination requires a focus on the mental nature of the rituals rather than solely behavioral aspects.
Cognitive Behavioral Therapy (CBT): CBT helps identify destructive thought patterns such as catastrophic thinking or overvalued ideation that fuel rumination. Therapy seeks to reframe distorted beliefs like “If I don’t analyze this thoroughly, I’ll make a grave error,” or “Having this thought means I’m a bad person.” Through cognitive restructuring and real-life behavioral tests, clients can challenge and validate these beliefs.
Exposure and Response Prevention (ERP): ERP for OCD of rumination is designed to diminish mental rituals. Since compulsions are often covert, such as reconsidering or analyzing, ERP necessitates inventive exposures that elicit rumination but prevent the associated mental response. Initial exposures might include allowing a triggering thought to surface while resisting the urge to replay it or check memories. Techniques like “thought surfing” or deliberate postponements where clients delay analysis for a set period help the mind recognize that anxiety can lessen without engaging in mental neutralization. The aim is to develop habituation, understanding that anxiety peaks but eventually subsides without rituals, gradually weakening the compulsion’s influence.
Acceptance and Commitment Therapy (ACT): complements CBT and ERP for OCD of rumination by shifting the relationship individuals have with their thoughts. ACT introduces cognitive defusion strategies perceiving thoughts as mere mental events rather than absolute truths and clarifies values so that actions are motivated by meaning rather than the need for certainty. For individuals experiencing moral rumination, ACT can aid in acknowledging intrusive doubts as “just thoughts” and choosing actions aligned with their values, such as mending relationships or pursuing meaningful work.
Wellness coaching: serves as an “upgrade principle” that enhances therapy outcomes and fosters daily resilience. Coaches assist clients in structuring routines that promote cognitive flexibility, such as ensuring consistent sleep, engaging in regular exercise, consuming nutritious foods, and implementing stress-reduction techniques like mindfulness or progressive muscle relaxation. Practical coaching might include time management strategies to curb excessive rumination, improving digital habits to alleviate cognitive overload, and planning activities to engage in meaningful pursuits.
Personality dynamics course correction: is also essential to correcting deeper patterns that perpetuate OCD of rumination. Many sufferers exhibit traits of perfectionism, hyper-responsibility, and uncertainty intolerance attributes that can convert normal reflection into pathological rumination. Therapy goes into the origins of these traits, which might stem from childhood expectations, cultural narratives, or internalized standards, and supports the process of rewriting internal interpretation. A healthier narrative can evolve from “I must achieve absolute certainty” to “I can make sound judgments with imperfect information.”
Developing healthy coping strategies: is practical and vital for facilitating daily changes. Instead of engaging in analytical loops, clients are taught grounding techniques, brief mindfulness exercises, and behavioral alternatives that interrupt the habit. Grounding exercises focus on activating the senses to redirect attention away from mental replay. Short breathing exercises or body scans can help lower the autonomic arousal associated with rumination. Behavioral substitutions might include “postponement” (designating a specific time for reflection), reality-testing (quickly assessing the evidence for and against a feared belief), and engaging in active problem-solving only when issues warrant it. Over time, these practices can become automatic, providing immediate alternatives to mental rituals.
Enhancing emotional and mental health: is woven throughout the recovery process since OCD of rumination often coexists with mood disturbances. Therapeutic efforts focus on sleep regulation, rekindling social connections, and planning activities to counter behavioral withdrawal. Peer support can offer validation and modeling; hearing others articulate similar mental struggles reduces feelings of shame and fosters hope. Family therapy helps loved ones understand how to respond without fueling reassurance cycles promoting supportive engagement without frequently answering repeated inquiries. Training in emotion regulation identifying triggers, labeling feelings, and employing grounding strategies equips clients to experience discomfort without resorting to compulsive resolutions.
Relpase management: Preventing relapse is essential, as OCD of rumination can fluctuate over time. Therapists guide clients in recognizing early signs such as prolonged thinking sessions, avoidance behaviors, or increased reassurance-seeking and employing booster strategies: reactivating ERP tasks, scheduling wellness check-ins, and utilizing coping scripts. Developing a written relapse prevention plan that outlines support systems, targeted exposures, and action steps can lessen panic when former patterns reemerge and bolster confidence in applying acquired skills.
Success Story – I
Rohini, a 29-year-old software developer, had always been thoughtful and analytical. But after a heated argument with a colleague, her reflection spiraled into relentless mental replay. She kept re-examining every word she had said, worrying that she might have been rude. What started as a harmless replay soon turned into a daily cyclen revisiting the memory on her commute, at work, and even while trying to sleep. Her mind questioned endlessly: “Did I sound arrogant? What if I hurt them?” The more she analyzed, the worse she felt.
When Rohini sought therapy at Emotion of life, she was diagnosed with OCD of rumination. Her treatment began with CBT to identify cognitive distortions like over-responsibility and catastrophizing. She learned how her urge to “solve” the thought was actually maintaining her anxiety. ERP helped her resist mental checking, she practiced allowing uncertainty about the argument without mentally replaying it. ACT introduced her to the concept of “defusion” seeing thoughts as passing events rather than facts demanding attention. Through wellness coaching, she rebuilt her daily routine, adding yoga, journaling, and limited “reflection windows” for structured thinking. Personality-focused work helped her soften her perfectionism and develop self-compassion.
Within three months, Rohini reported significant improvement. Her rumination time dropped from hours to minutes. By six months, she could recall the same memory without spiraling into analysis. “My mind still questions things,” she said, “but now I choose which ones to answer.” Rohini’s recovery symbolizes how structured therapy and lifestyle upgrades can free the mind from the cycle of mental over-analysis.
Success Story – II
Meghna, a 32-year-old philosophy lecturer, began experiencing intrusive existential thoughts after her father’s death. Questions like “What’s the point of life?” and “How can we know anything for sure?” started consuming her days. She spent hours researching online, reading spiritual texts, and analyzing theories but the answers only created new doubts. Her students noticed her distraction, and sleep became nearly impossible.
After evaluation, Meghna was diagnosed with existential rumination OCD. Her therapist explained that her thoughts were not philosophical curiosity but obsessive loops fueled by anxiety and uncertainty. The first stage of treatment involved ERP exercises: intentionally reading philosophical paradoxes and resisting the urge to “solve” them. This was deeply uncomfortable at first, but it taught her that uncertainty could coexist with peace. Through ACT, she learned to accept doubt as part of human experience, focusing on living her values rather than resolving unanswerable questions. Her wellness coaching sessions encouraged grounding in daily experiences: gardening, slow breathing, and mindful walks. Personality dynamics work revealed her lifelong drive for control and intellectual perfection, which she gradually learned to relax.
Over time, Meghna’s rumination frequency decreased dramatically. She described a newfound ability to experience awe without anxiety reading philosophy not to “fix” her mind but to appreciate it. “I don’t need all the answers anymore,” she shared in her final session. “I just need to live fully.” Today, Meghna balances her intellectual passion with emotional wisdom, embodying the essence of recovery from OCD of rumination.
1. What is OCD of rumination?
OCD of rumination is a form of obsessive-compulsive disorder where a person gets trapped in repetitive thinking loops. These thoughts are intrusive, distressing, and feel impossible to stop. Unlike normal reflection or problem-solving, rumination OCD feels uncontrollable and offers no resolution.
2. How is rumination OCD different from overthinking?
Overthinking usually involves conscious worry or planning, while rumination OCD feels intrusive, unwanted, and driven by anxiety. Overthinkers can pause or redirect thoughts, but people with OCD of rumination feel mentally “stuck,” unable to stop replaying or analyzing scenarios despite knowing it’s unhelpful.
3. What are the common symptoms of OCD of rumination?
Common symptoms include repetitive mental replay of events, analyzing “what-if” scenarios, excessive guilt, moral or existential doubts, relationship obsession, and an inability to focus due to mental loops. People often feel mentally exhausted and trapped in their thoughts for hours.
- Can rumination be a form of mental compulsion?
Yes. In OCD of rumination, the act of mentally analyzing or replaying events becomes a compulsion. It’s a way of seeking certainty or relief from anxiety. Unfortunately, this relief is temporary, and the cycle strengthens the disorder over time
- When should I seek professional help for rumination OCD?
You should seek help if repetitive thoughts consume more than an hour per day, interfere with daily functioning, or cause distress, guilt, or indecision.
Conclusion
If you believe OCD of rumination is significantly affecting your life, if persistent intrusive thoughts and endless mental checking consume an hour or more each day, disrupt your sleep, or damage relationships reaching out to Mr. Shyam Gupta, experienced in treating OCD is a crucial step. With targeted CBT and ERP tailored for mental compulsion, ACT to reshape your relationship with your thoughts, wellness coaching to enhance daily resilience, personality-focused work to adjust rigid beliefs, and practical coping techniques to supplant rituals, you can regain mental clarity and agency. Recovery doesn’t mean never questioning again; it’s about choosing how to live alongside those questions. Seeking help is the brave first step towards reducing rumination and embracing a fuller life.
Call: +91 9368503416 www.emotionoflife.in Email: info@emotionoflife.in
Book Now | Review | OCD Types | Our Experts | Success Stories| Contact Us| MyPsychologist