Confession OCD
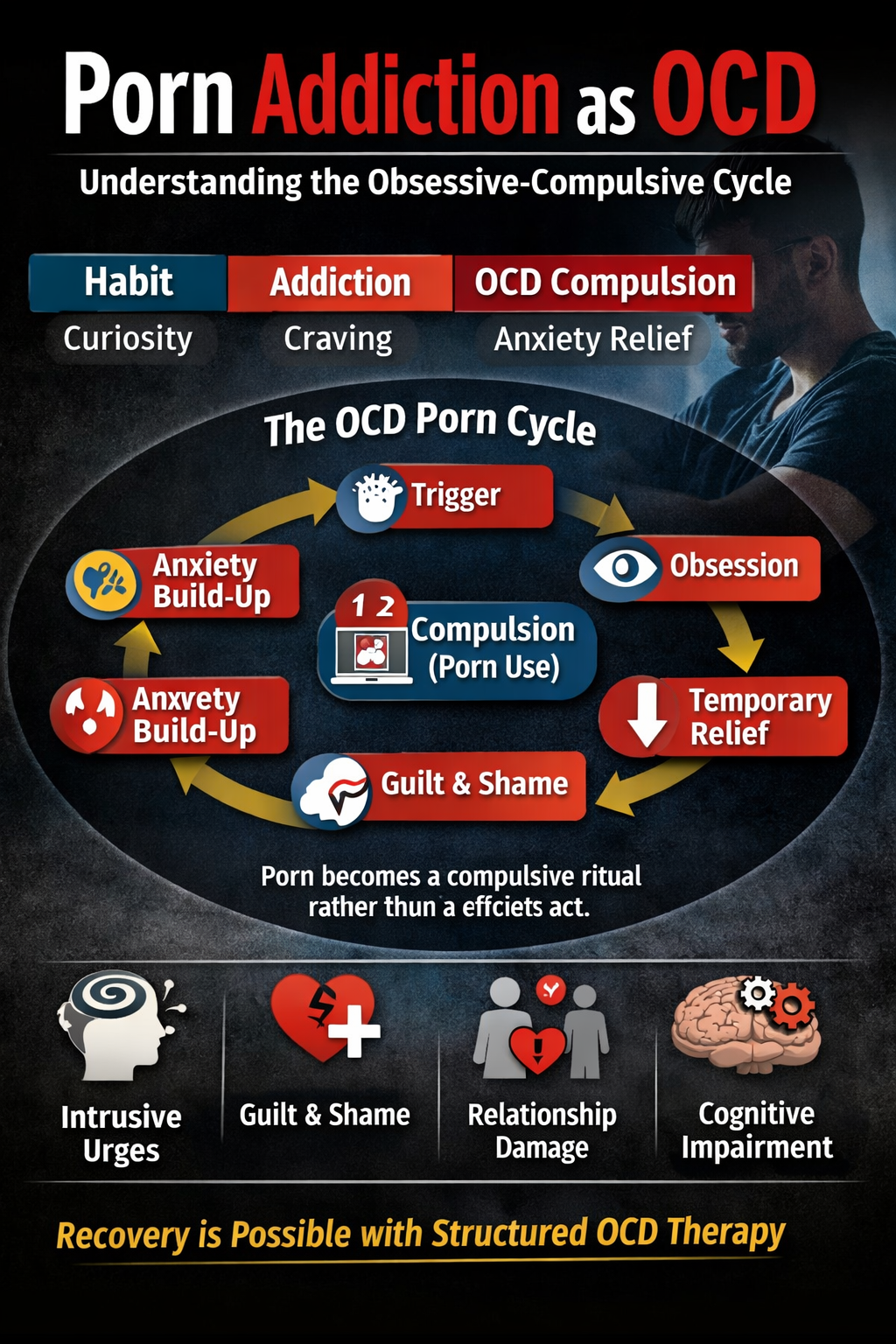
Confession OCD is a subtype of obsessive-compulsive disorder marked by intrusive, distressing thoughts (obsessions) and a compulsive urge to confess or seek reassurance. These thoughts often revolve around perceived moral, ethical, or religious transgressions—even when no actual wrongdoing has occurred.
Obsessions in Confession OCD
Common obsessions include:
- Fear of having hurt someone (physically or emotionally)
- Worries about lying, being dishonest, or sinning
- Intrusive thoughts of violence, sexuality, or blasphemy
- Concerns about violating religious or moral codes
Types of Obsessions in Confession OCD
- Scrupulosity – Obsessions about moral/religious perfection
- Harm OCD – Fears of unintentionally causing harm
- Taboo Thoughts – Intrusive thoughts about socially unacceptable topics
Compulsions in Confession OCD
Compulsions are mental or physical acts used to reduce distress:
- Compulsive confession to friends, religious figures, or therapists
- Reassurance seeking to validate moral integrity
- Avoidance of triggering situations (e.g., religious discussions)
- Mental rituals, such as prayer or repeating phrases
These behaviors offer temporary relief but reinforce the OCD cycle over time.
Symptoms in Confession OCD
- Intrusive, unwanted thoughts
- Intense guilt, shame, and anxiety
- Repeated confessions and reassurance seeking
- Excessive rumination and moral self-analysis
- Impaired functioning at work, school, or in relationships
- Fear of judgment or rejection
- Difficulty recognizing these thoughts as OCD (poor insight)
Impact of Confession OCD on Daily Life
- Disrupts concentration and job performance
- Strains relationships due to constant confessing or validation needs
- Leads to isolation, depression, and avoidance of social or religious activities
- Creates feelings of hopelessness and low self-worth
Causes and Risk Factors of Confession OCD
- Genetics and family history
- Neurobiological factors (serotonin imbalance)
- Personality traits like perfectionism or moral rigidity
- Cultural/religious upbringing emphasizing purity or guilt
- Childhood trauma or emotionally intense religious experiences
Treatment Approaches for Confession OCD
Cognitive-Behavioral Therapy (CBT)
- Exposure and Response Prevention (ERP): Facing triggering thoughts without confessing.
- Cognitive Restructuring: Challenging distorted beliefs about morality and guilt.
Mindfulness and Acceptance and Commitment Therapy (ACT)
- Observing intrusive thoughts without acting on them.
- Learning to accept discomfort and uncertainty without seeking reassurance.
Correcting Personality Dynamics
- Reducing sensitivity and over-responsibility.
- Improving emotional regulation and resilience.
Lifestyle and Emotional Health
- Balanced nutrition and healthy sleep routine.
- Building emotional resilience and practicing stress reduction techniques.
- Educating family members on how to support recovery without enabling compulsions.
Case Studies of Confessional OCD
Case Study 1: Sarah, 30 years old
Background: Sarah grew up in a devoutly religious family, emphasizing moral perfection.
Symptoms: Persistent intrusive thoughts about sinning or offending God, leading to repeated confessions and prayers.
Impact: Difficulty focusing at work, social withdrawal, strained relationships due to excessive reassurance seeking.
Treatment: Through CBT and ERP, Sarah learned to face her intrusive thoughts without confessing and restructured her beliefs about morality. She gradually reduced her compulsion to confess and regained emotional peace.
Case Study 2: Ahmed, 25 years old
Background: Ahmed, from a conservative religious community, struggled with guilt and fear of blasphemy.
Symptoms: Intrusive doubts about moral impurity and salvation; compulsive praying and ritual performance.
Impact: Panic attacks, social withdrawal, and difficulty maintaining daily routine.
Treatment: Ahmed underwent culturally sensitive therapy integrating CBT, ERP, and religious understanding. Over time, he learned to challenge irrational guilt and regain control over his thoughts and emotions.
16 Steps of OCD Recovery – Emotion of Life
- Awareness of OCD patterns
- Understanding the OCD cycle
- Accepting intrusive thoughts as harmless mental events
- Identifying triggers
- Learning ERP principles
- Gradual exposure to fears
- Preventing compulsive confessions
- Practicing mindfulness
- Challenging irrational beliefs
- Improving emotional regulation
- Enhancing problem-solving skills
- Building self-compassion
- Strengthening social connections
- Maintaining a healthy lifestyle
- Relapse prevention planning
- Celebrating recovery milestones
Call: +91 9368503416 www.emotionoflife.in Email: info@emotionoflife.in
Book Now | Review | OCD Types | Our Experts | Success Stories| Contact Us| MyPsychologist