Cognitive Behavioral Therapy for OCD is a mental health condition where individuals experience frequent, distressing thoughts called obsessions and feel driven to perform certain routines or behaviours known as compulsions to manage the anxiety these thoughts bring. Although these behaviours may seem to ease discomfort briefly, they usually reinforce fear and make symptoms worse over time. Cognitive Behavioural Therapy (CBT) is a focused, practical approach used to help people manage their thoughts, feelings, and actions. It is widely recommended as one of the most effective psychological therapies for those living with OCD.
How Cognitive Behavioral Therapy for OCD Helps People with OCD
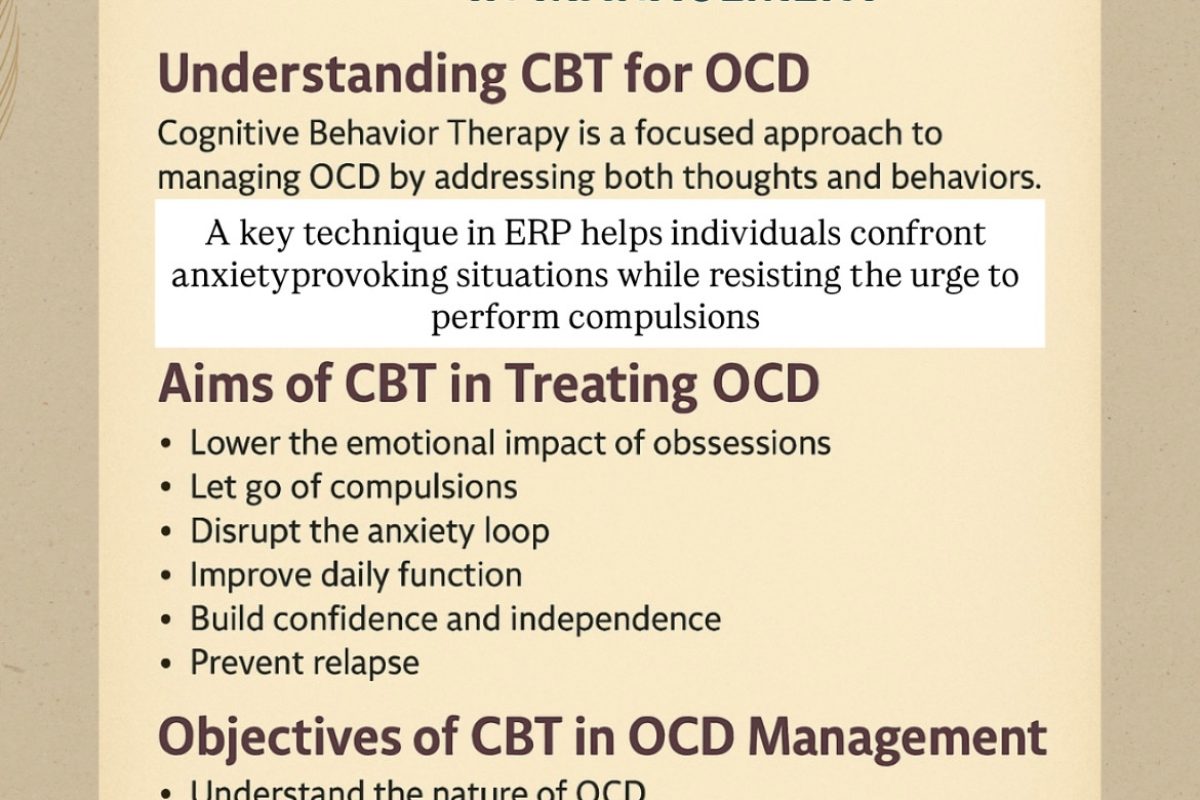
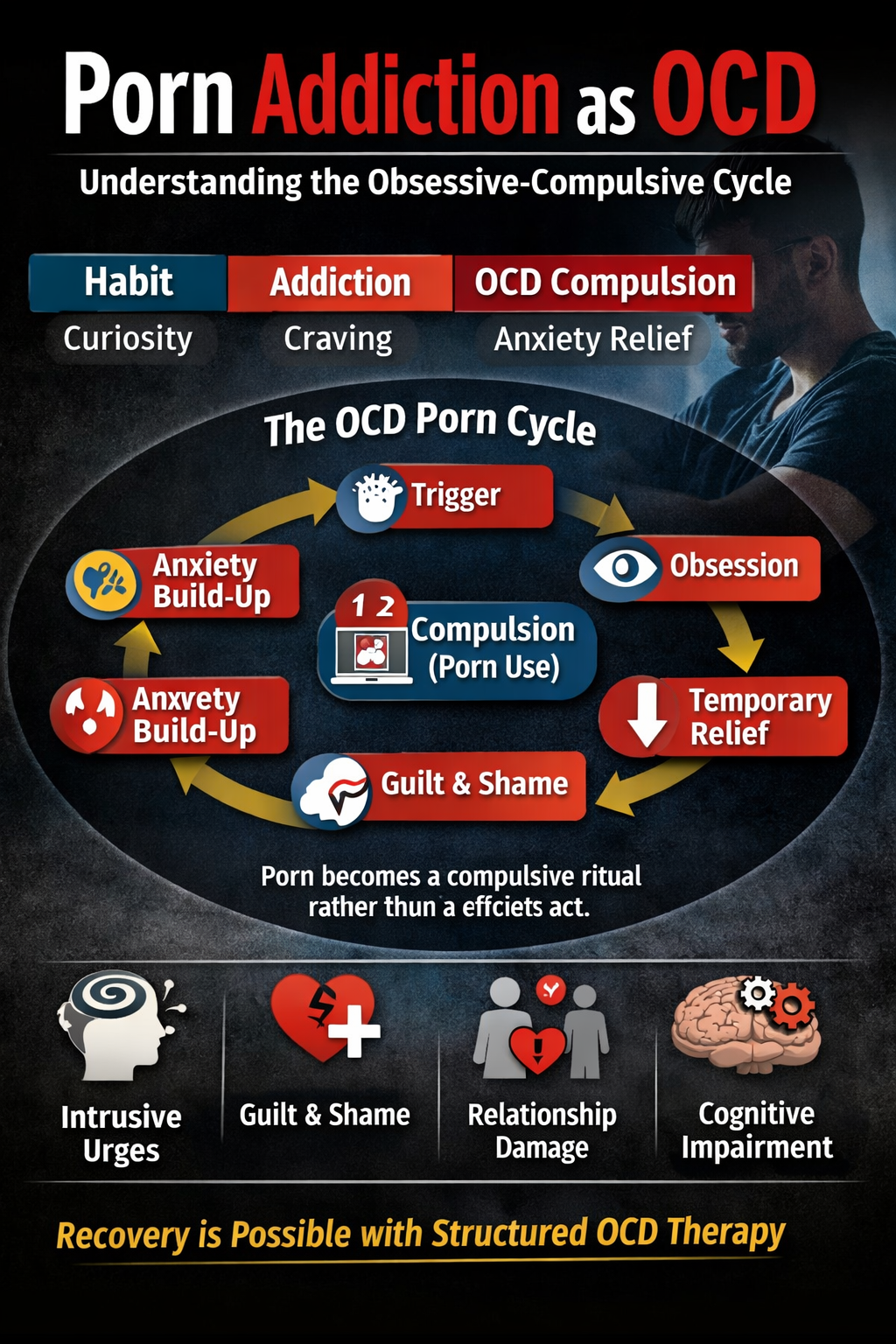
Cognitive Behavioral Therapy for OCD is built on the concept that our thoughts influence how we feel and behave. For someone with OCD, a thought might be misread as dangerous, even if there is no real threat. For instance,a person might worry that something bad will happen if they don’t check a door lock several times or wash their hands repeatedly. CBT for Obsessive Compulsive Disorder helps individuals notice these patterns and change how they respond. Instead of giving in to rituals, people learn to tolerate uncertainty and accept that not acting on a thought doesn’t lead to disaster. Over time, they gain more control and experience fewer urges to engage in compulsive actions. A key technique used within CBT for Obsessive Compulsive Disorder is Exposure and Response Prevention (ERP). ERP involves slowly and safely facing anxiety-provoking situations without performing the usual rituals. As individuals repeat this process, their anxiety gradually decreases, and they build confidence in resisting compulsions.
Aims of Cognitive Behavioral Therapy for OCD in Treating OCD
The ultimate goal of CBT for Obsessive Compulsive Disorder treatment is to help people overcome the cycle of obsessive
thinking and compulsive behaviour. This involves several important aims:
1. Lowering the Emotional Impact of Obsessions Helping individuals realise that thoughts
alone are not dangerous and do not require a reaction.
2. Letting Go of Compulsions Encouraging people to stop rituals that they believe protect them
but are actually part of the problem.
3. Disrupting the Anxiety Loop Breaking, the repeated cycle where obsessions lead to
temporary relief through rituals, which in turn reinforce the fear.
4. Improving Daily Function Supporting individuals in living their everyday lives working,
studying, socialising without OCD limiting their ability.
5. Building Confidence and Independence Helping people feel strong and capable of managing
anxiety without relying on compulsions or reassurance.
6. Preventing Relapse Giving individuals tools and strategies to cope with future stress or triggers, so they can maintain progress after therapy.
Objectives of Cognitive Behavioral Therapy for OCD in OCD Management
To achieve these goals, Cognitive Behavioral Therapy for OCD follows a structured path with clear, practical steps:
1. Understanding the Nature of OCD Therapy starts by explaining how OCD works how certain
thoughts become stuck and lead to ritualised behaviour. This understanding helps reduce shame and confusion.
2. Recognising Personal Triggers, the therapist helps the individual identify what kinds of
situations or thoughts trigger anxiety and compulsive responses.
3. Challenging Unhelpful Thinking People are guided to notice extreme or irrational thoughts
for example, believing that harm will come if they don’t follow a ritual and to consider more
balanced alternatives.
4. Changing Thought Patterns Individuals learn how to shift from fear-driven reactions to more
flexible and realistic thinking.
5. Creating a Personal Challenge list is built least to most intense fear in which person works
through them in order CBT also teaches healthy ways to manage anxiety, such as relaxation
techniques, mindfulness, and breathing exercises.
6. Making a Long-Term Maintenance Plan Toward the end of therapy, the focus shifts to
creating a strategy for recognising early signs of difficulty and preventing setbacks in the
future.
Case Example:
Rohan’s Recovery Path Rohan, a 22-year-old college student, struggled with intrusive thoughts
about accidentally hurting people, even though he never intended to. As a result, he avoided
sharp objects and even kept his distance from others. This avoidance made issues in his daily
life and studies.During CBT sessions, Rohan learned that having a thought doesn’t mean he
will act on it. With his therapist, he slowly started facing his fears, first by holding safe objects
and eventually by sitting close to others. Over time, his anxiety reduced, and his confidence
grew. By the end of therapy, Rohan had resumed his normal routines and was no longer
governed by fear.
Tips for Successful Cognitive Behavioral Therapy for OCD
• Begin treatment as early as possible, as addressing OCD symptoms promptly makes it easier
to interrupt and change unhealthy behaviour patterns.
• Work with a Qualified Therapist: A therapist trained in OCD and ERP can guide the process
more effectively.
• Stay Committed: Regular sessions and following through with home tasks are essential.
• Include Support: Involving family or friends who understand the process can be beneficial.
• Be Patient with Progress: Improvement takes time, and small steps lead to big changes.
Conclusion on Cognitive Behavioral Therapy for OCD
Cognitive Behavioural Therapy is a powerful, practical tool for those dealing with OCD.
Rather than trying to eliminate every unwanted thought, CBT teaches individuals how to
respond differently without fear or compulsions. By learning to face discomfort, delay rituals,
and accept uncertainty, individuals can break the OCD cycle. With consistent effort, expert
guidance, and the right mindset, it is entirely possible to move toward a more peaceful and
fulfilling life.
Call: +91 9368503416 www.emotionoflife.in Email: info@emotionoflife.in
Book Now | Review | OCD Types | Our Experts | Success Stories| Contact Us| MyPsychologist