Aphantasia OCDa person with aphantasia OCD, a lesser-known type of obsessive-compulsive disorder, becomes fixated on their incapacity to construct mental images or continuously assesses if they can visualize anything correctly. Aphantasia is not a disorder in and of itself, but when OCD takes hold of it, it turns into a vicious cycle of anxiety, uncertainty, excessive checking, and mental tiredness.
Aphantasia OCD occurs when a person becomes obsessively focused on their visual imagination abilities. Some people naturally have difficulty forming mental images, and some can visualize clearly, both are normal.
What does the person do?
The person constantly checks their mind’s eye
They compare their visualization to others
They fear something is “wrong” with their brain
They feel anxious when their imagination doesn’t work “perfectly.”
They repeatedly test their ability to visualize faces, shapes, objects, and scenes.
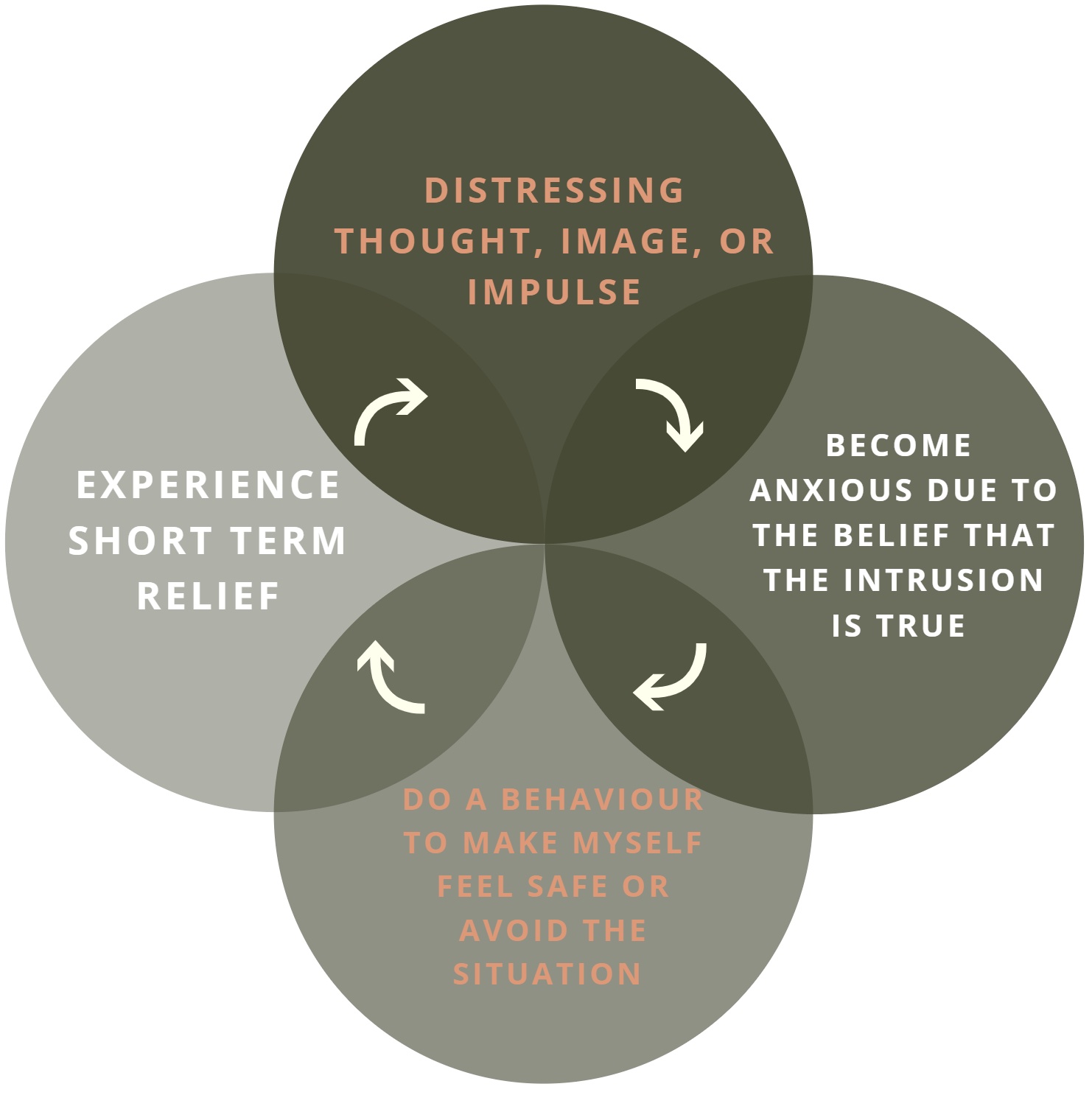
The vicious cycle
Obsessive thought → anxiety → checking visualization → temporary relief → more obsession.
Aphantasia OCD Symptoms
Psychological Symptoms
Intrusive thoughts about not being able to visualize
Constant self-testing (“Can I imagine an apple? A tree? A face?”)
Fear of “mental decline” or “brain damage”
Comparing one’s mental imagery with others
Obsessive reading about aphantasia
Feeling guilty or scared when visualization fails
Endless mental effort trying to “push” the imagination
Fear that life will lose meaning without visualization
Overthinking every internal experience
Physiological symptoms
Chest tightness
Fast heartbeat while monitoring episodes
Sleep difficulties, exhaustion from mental overwork, and headaches from intense focus
Anxiety-related appetite loss
Pacing or restlessness
Breathing shallowly
Aphantasia OCD types
OCD Visualization Checking
Testing mental imagery repeatedly: “Can I visualize a circle? How about a home?
This checking turns into an obsession.
OCD with Existential Aphantasia
Fear that life is “less meaningful,” “less genuine,” or “empty” because one cannot visualize
Aphantasia OCD Associated with Memory
Fearing that a lack of mental images may cause them to lose their identity, loved ones, or past experiences
OCD, Aphantasia, and Health Anxiety
Fear that altered mental images indicate neurological problems, dementia, or brain damage.
Comparative OCD Aphantasia
Comparing oneself to others all the time: “How clearly can they view things in their mind? Why not me?
Excessive Focus on Internal Experience
Hyper-awareness of internal sensations, continually observing the mind instead of using it naturally.
Aphantasia OCD Causes
Psychological Causes
Increased consciousness of one’s own experiences
Uncertainty intolerance (“What if this gets worse?”
Perfectionism and overanalyzing
Fear of losing mental control
Inclination to examine each feeling or concept
Ruminating behaviors that exacerbate the OCD cycle
Social Causes
Listening to people discuss their vivid imaginations
Reading papers or watching videos that discuss “perfect visualization”
Comparing oneself to influential people or peers
Pressure to be “visual” or “creative” at work or in the classroom
Environmental Causes
Stressful times that lead to intrusive thoughts
Sleep deprivation or burnout
Overindulgence in mental health content
Abrupt emotional shifts
Inadvertent triggers that change focus within the mind, such as mindfulness practices or meditation
Aphantasia OCD Treatment
Psychoeducation
The first and most crucial stage in treating Aphantasia OCD is psychoeducation. Here, the person discovers that aphantasia is not an indication of brain damage, memory loss, or mental deterioration, but rather a typical variance in human experience. Many folks function perfectly fine and have less vivid or non-existent visuals by nature. Anxiety dramatically decreases when a person realizes that their dread is caused by OCD rather than a real brain issue. This information aids in ending the loop of miscommunication and anxiety that sustains OCD.
Cognitive Behavioural Therapy (CBT)
CBT helps individuals identify and challenge irrational beliefs related to visualization. People often believe that they “must visualize clearly,” or that “not seeing images means something is wrong.” CBT reframes these thoughts into realistic interpretations, reducing the mental pressure that fuels OCD. Through structured exercises, the individual learns that unclear or weak imagery is not harmful and that their thoughts are not indicators of danger. This shift in beliefs reduces anxiety and gives the person more control over their reactions.
Exposure and response prevention (ERP)
ERP is a potent therapeutic approach in which the patient learns to cease engaging in compulsive behaviors, such as continuously reviewing their visualization, examining their mental images, or looking for assurance. Rather, they experience the anguish of “not knowing” or “not checking.” The brain eventually learns that reducing checking has no negative effects. As a result, the OCD cycle is weakened, and the person is better able to handle uncertainty. Anxiety naturally decreases as intrusive thoughts lose their strength and compulsions diminish.
Wellness coaching
The management of OCD symptoms is significantly influenced by lifestyle factors. In order to settle the mind and lessen intrusive thoughts, it is beneficial to get enough sleep, limit screen time, engage in regular physical activity, and establish regular daily routines. A healthy environment for healing is produced by stress-reduction strategies like breathing exercises, grounding exercises, and less overthinking. Therapy works considerably better when the body is in balance because the mind is less reactive. Long-term recovery is strengthened by these helpful adjustments.
Social Skill Training
People with Aphantasia OCD benefit from social skills training when their compulsive attention to internal events starts to interfere with their social interactions. Because they are obsessed with their thoughts, anxious about their ability to visualize things, or afraid of becoming distracted during talks, many people with this subtype retreat socially. By providing useful techniques for maintaining conversations, expressing emotions, and staying grounded in the outside world rather than the mind, SST helps rebuild confidence. To maintain relationships, this program teaches effective communication, eye contact, facial expressions, and active listening.
When people use these techniques, their focus automatically shifts from internal checks to actual encounters. This lessens self-monitoring, comparison, and rumination, all of which are essential elements that sustain Aphantasia OCD. Social Competencies, moreover, the training helps in ending the isolation cycle, which frequently leads to an increase in intrusive thoughts. People’s brains relearn that exterior life is more significant than mental imagery when they re-engage in talks, relationships, and everyday social activities. Over time, this helps the person feel more present, balanced, and connected while also boosting confidence and lessening the severity of OCD symptoms.
Aphantasia OCD Success Stories
1. Rhea, 21 – College Student (Mumbai, India)
Rhea developed Aphantasia OCD during her second year of college when she suddenly became hyper-aware of her inability to visualize objects clearly. She spent hours trying to imagine faces and scenes, and eventually started avoiding friends because she feared she would zone out during conversations. This isolation increased her checking behaviour and made her more anxious.
Through therapy, she learned that her intrusive thoughts were harmless and part of OCD. Social Skills Training helped her re-engage with group discussions, practice active listening, and reconnect with friends without getting stuck inside her mind. Over three months, her compulsive checking reduced significantly, and she began participating confidently in classroom activities. She now understands that clear mental images are not necessary for meaningful social interaction, and her anxiety levels have dropped by nearly 80%.
2. Aarav, 28 – Graphic Designer (Bangalore, India)
Aarav struggled with Aphantasia OCD after watching an online video about “visual thinkers.” He began obsessively comparing his ability to visualize with others and feared losing his creativity. He became socially withdrawn, avoiding discussions at work and feeling disconnected from colleagues. His self-confidence dropped, and he spent most of his time analysing his mental images instead of engaging with the world around him.
With Cognitive Behavioural Therapy and Social Skills Training, Aarav learned to shift attention outward, participate actively in small talk, and stay present during meetings. Practicing these skills daily helped him break his habit of internal monitoring. As his social interactions improved, his obsessions about visualization reduced naturally. Today, Aarav maintains healthy relationships at work, collaborates confidently with his team, and no longer checks his mental imagery throughout the day.
3. Sara, 34 – School Teacher (Toronto, Canada)
Sara experienced Aphantasia OCD after a stressful period in her job. She noticed that her mental images were unclear and immediately feared that she was developing a cognitive disorder. This fear made her retreat from social interactions, constantly analyzing her thoughts and avoiding conversations where she felt distracted. She struggled with guilt and loneliness, believing she was “not present enough” for her students or colleagues.
Therapy helped her understand that OCD—not visual impairment—was the problem. Through Social Skills Training, she relearned conversational grounding techniques such as maintaining eye contact, asking follow-up questions, and focusing on external details instead of internal sensations. By gradually rebuilding her confidence in social environments, she was able to reduce overthinking and reconnect with her students and friends. Her anxiety reduced by half within two months, and she now lives without the fear of losing her imagination.
Client Reviews
1. Mehak, 24 – Psychology Student, Delhi
“I joined Emotion of Life during a phase where intrusive thoughts were taking over my day. The step-by-step structure and practical exercises helped me understand my mind without fear. Within weeks, I felt more in control and less overwhelmed. I’m finally getting back to studying with confidence.”
2. Rohan, 30 – Software Engineer, Pune
“Emotion of Life gave me clarity that no amount of Googling ever did. The therapist helped me break my compulsions slowly and consistently, and the sessions felt genuinely human. For the first time in years, I’m seeing real changes in my daily behaviour and thinking patterns.”
3. Sana, 28 – Fashion Designer, Mumbai
“I used to feel stuck inside my own head all the time. The techniques taught at Emotion of Life helped me shift attention outward and reconnect with my work. I’m more present, calmer, and the intrusive loops have reduced so much. I’m grateful for the consistent guidance.”
4. Aditya, 35 – Marketing Professional, Hyderabad
“The best part of Emotion of Life was that the approach was simple and doable. No complex jargon—just clear steps that worked when I practiced them. My anxiety reduced steadily, and I no longer panic when intrusive thoughts show up. This program has been life-changing.”
5. Nisha, 27 – Graduate Student, Chandigarh
“My OCD made me doubt everything about myself. The therapist at Emotion of Life taught me how to understand my thoughts instead of fighting them. The improvement has been gradual but very real. I’m more confident, less reactive, and my compulsions have reduced drastically.”
AT Emotion of Life, we follow a thorough 16-step process to ensure complete recovery and relapse management
1. Awareness – Understanding OCD is a fear-based disorder.
2. Understanding Intrusive Thoughts – Learning that thoughts are harmless.
3. Identifying Triggers – Noticing situations that activate counting.
4. Writing Ritual Patterns – Understanding your habits.
5. Separating Thoughts & Identity – Knowing “You are not your thoughts.”
6. Breaking Attention Cycle – Training yourself not to react to urges.
7. Reducing Safety Behaviours – Slowly cutting down rituals.
8. Exposure Sessions – Facing situations without counting.
9. Response Prevention – Resisting the urge to complete the ritual.
10. Sitting with Discomfort – Allowing anxiety to naturally come down.
11. Restructuring Beliefs – Learning that numbers do not control reality.
12. Building Behavioural Flexibility – Doing things imperfectly on purpose.
13. Strengthening New Habits – Repeating healthier responses.
14. Relapse Prevention – Preparing long-term coping strategies.
15. Lifestyle Balancing – Regulating sleep, food, movement, and routine.
16. Living Authentically – Returning to normal life without rituals.
Conclusion
When the mind gets too preoccupied with interior sensations like visualization, aphantasia OCD can feel overwhelming and perplexing. However, when properly recognized, the disease is quite controllable. People can progressively interrupt the cycle of checking and fear with the correct combination of psychoeducation, CBT, ERP, metacognitive practice, attentional redirection, and supportive routines. Social skills training also helps by reestablishing confidence, lowering feelings of loneliness, and rooting them in real-life interactions rather than internal monitoring. Consistent practice, guided approaches, and a caring therapy approach—like the one provided at Emotion of Life, all contribute to genuine healing, as demonstrated by numerous success stories. People can reclaim a sense of normalcy, connection, and balance by learning to live freely without worrying about how their minds “should” function with the correct tools and patience.
Contact: Email: info@emotionoflife.in
Phone/WhatsApp: 9368503416 Call for Initial Discussion
Emotion of Life — OCD Treatment, Research & Training Institute. Lead Specialists: Shyam Gupta & Pratibha Gupta. We treat 70+ OCD subtypes and specialize in complex, chronic, and treatment-resistant cases. Non-medication recovery using CBT, ERP, and holistic wellness integration.
Book Now |Review |OCD Types |Our Experts |Success Stories|Contact Us|
MyPsychologist