Something bad may happen in OCD article provides a complete, expert-level exploration of this subtype, its psychological mechanisms, common triggers, symptoms, and effective treatment pathways—especially non-pharmacological approaches including the Emotion of Life 100 Days 100 Sessions OCD Recovery Program.
What Is “Something Bad May Happen” OCD?
Something Bad May Happen OCD This subtype is characterized by an exaggerated sense of danger and a persistent belief that one must stay hyper-alert to prevent catastrophic outcomes. The brain remains in a state of threat-surveillance, making harmless situations feel unsafe.
Core Features Include in “Something Bad May Happen” OCD:
- Intrusive thoughts predicting disaster (accident, illness, loss, harm)
- Inflated sense of responsibility (“If I don’t check, something bad will happen”)
- Catastrophic misinterpretation of normal sensations or thoughts
- Compulsive behaviors to prevent imagined harm
Even when logically knowing the fear is unrealistic, the emotional intensity feels overwhelming.
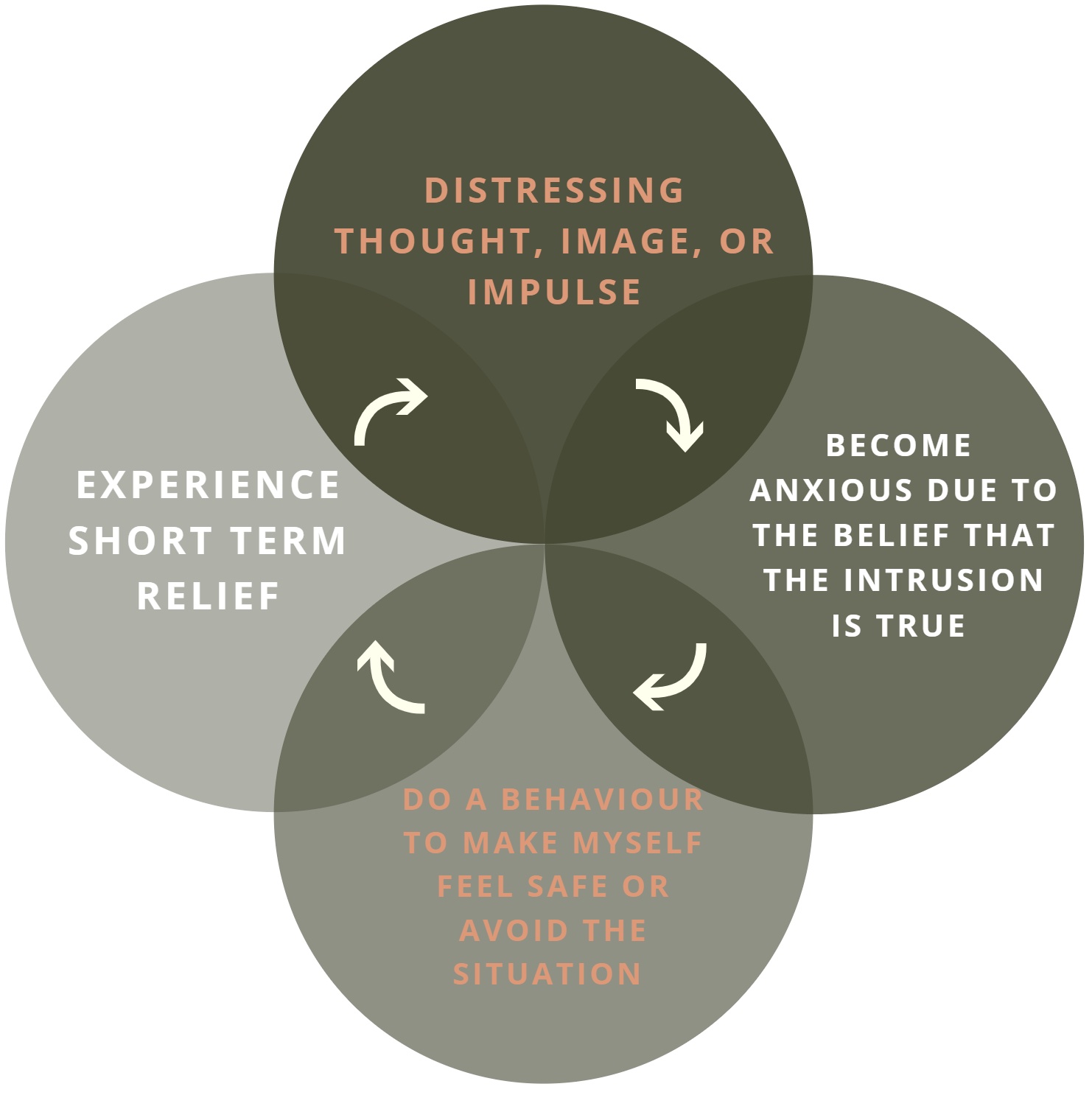
Why Do These Thoughts Occur? Over analysis of situation at cognitive level and processing as psychological phenomena creates a constant feeling of “something is wrong” even when everything is fine.
Over-Responsibility Schema: Individuals believe they must prevent all possible harms even events outside their control.
Catastrophic Thinking Loop: Normal thoughts are misinterpreted as warnings, leading to compulsions for relief.
Difficulty Trusting Reality: The brain demands certainty where certainty is impossible, creating chronic anxiety.
Common Intrusive Thoughts in “Something Bad May Happen” OCD
Themes Include:
- “If I don’t check the door, my family may be harmed.”
- “If I say something wrong, I may cause a disaster.”
- “If I leave the house, an accident may happen.”
- “If I don’t pray or repeat a ritual, something bad will occur.”
- “If I ignore a thought, it may become reality.”
These thoughts feel urgent, threatening, and morally significant—even though they are just mental events.
Symptoms of “Something Bad May Happen” OCD
Cognitive Symptoms in “Something Bad May Happen” OCD
- Catastrophic thinking
- Overestimation of threat
- Fear of losing control
- Persistent mental rehearsal of worst-case scenarios
Emotional Symptoms in “Something Bad May Happen” OCD
- High anxiety
- Guilt and shame
- Fear of responsibility
- Hypervigilance
Behavioral Symptoms in “Something Bad May Happen” OCD
- Compulsive checking (locks, appliances, actions)
- Asking for reassurance repeatedly
- Avoiding situations linked with fear
- Neutralizing thoughts or rituals
- Monitoring surroundings constantly
Triggers for “Something Bad May Happen” OCD
Common triggers include:
- Media news about accidents or crimes
- Sudden sounds or movements
- Ambiguous events or incomplete tasks
- Past mistakes or minor incidents
- Decision-making situations
- Fear of losing loved ones
How “Something Bad May Happen” OCD Differs from Rational Caution
Healthy caution is: Proportionate, Flexible, Based on reality, Ends when safety is confirmed,
OCD-driven fear is: Excessive, Rigid, Disconnected from reality, Never satisfied.
In OCD, the problem is not danger—it’s the mind’s interpretation of danger.
Compulsions That Maintain the Disorder as “Something Bad May Happen” OCD
Compulsions initially reduce anxiety but reinforce the brain’s belief that danger is real.
Common Compulsions in “Something Bad May Happen” OCD:
- Checking locks, switches, appliances repeatedly
- Replaying events mentally to confirm safety
- Seeking reassurance from family or therapists
- Avoiding responsibilities or decisions
- Performing rituals to “prevent” harm
Evidence-Based Treatment Approaches to Treat “Something Bad May Happen” OCD
1. Exposure and Response Prevention (ERP)
The gold standard therapy. ERP gradually exposes individuals to feared thoughts while blocking compulsions, teaching the brain that the fear is false.
2. Cognitive Behavioural Therapy (CBT)
Corrects catastrophic misinterpretations and responsibility distortions.
3. Mindfulness-Based Cognitive Therapy
Helps individuals observe intrusive thoughts without reacting or interpreting them as danger.
4. Dialectical Behaviour Therapy Skills
Especially useful for emotional regulation and tolerance of uncertainty.
5. Non-Medicine Holistic Approaches
These include lifestyle, behavioural, sensory, habit rewiring, and structured exposure models that help recalibrate threat perception without pharmacology.
Emotion of Life: Innovative Non-Medicine OCD Recovery Approach
Emotion of Life offers a structured, intensive, non-medicinal recovery model tailored for severe OCD cases, including catastrophic OCD.
Key Features of the Program:
- 100 Days – 100 Sessions – Intensive Recovery Model
- 360° Holistic Care Framework
- Behavioural rewiring and non-pharmacological intervention system
- Global access via online therapeutic ecosystem
- Individualized roadmap focusing on exposure, cognitive restructuring, and resilience building
This structured program has supported many individuals in overcoming severe intrusive fear patterns and regaining functional clarity.
Success Insight Example (Generalized, Non-Identifying)
Clients with catastrophic OCD often start therapy overwhelmed by fears that “something terrible will happen if I stop checking or take a risk.” Through systematic exposure, cognitive processing, and emotional reintegration, they learn to trust their internal sense of reality again. This therapeutic transformation is at the core of the Emotion of Life model. Team Structure for Managing 1 OCD Client in Emotion of Life, aligned with your existing therapy and recovery workflow. This format can be used for internal SOP, website, presentation, or client orientation.
Emotion of Life – Team Structure for One Client
Each client receives a 360° Recovery & Cure Support System, built around CBT + ERP + Lifestyle Re-Training and Daily Accountability.
Core Team Roles
| Role / Team Member | Key Responsibility | Frequency |
| Lead OCD Specialist Therapist (Shyam Gupta) | Case formulation, ERP progression, mindset restructuring, breakthrough guidance. | 3 sessions/week + weekly review meeting |
| CBT / ERP Co-Therapist (Trained Clinical Psychologist) | Daily ERP supervision, exposure planning, homework review, journaling tracking. | 2 Alternate Day Sessions |
| Wellness & Lifestyle Coach | Breathwork, nervous system regulation, grounding exercises, sleep & routine stabilization. | 1 times/week |
| Client Support Coordinator / Accountability Coach | Ensures follow-through, checks compliance, activity reminders, emotional support. | Daily WhatsApp/Text Check-ins |
| Program Director / Case Supervisor (Pratibha Gupta) | Quality assurance, case monitoring, relapse prevention planning, special cases review. | Bi-Weekly or On-Need Basis |
How the Team Collaborates (Workflow)
- Initial Assessment & Case Formulation
- Lead Therapist + Program Director jointly structure recovery blueprint.
- ERP & CBT Execution
- Co-Therapist delivers step-by-step exposures + cognitive restructuring tasks.
- Daily Accountability Tracking
- Support Coordinator ensures completion and consistency.
- Lifestyle & Emotional Strengthening
- Wellness Coach trains body-mind stability & stress regulation practices.
- Weekly Review Meeting
- Internal team sync to track progress, challenges, next-step plan.
- Monthly Phase Upgrade
- Lead Therapist updates therapy difficulty level based on client progress.
Communication Channels
| Purpose | Medium |
| Therapy Sessions | Google Meet / Zoom |
| Daily Check-ins | |
| Progress Monitoring | Shared ERP Sheets & Daily Routine Sheets |
| Emergency Emotional Support | On-call within defined boundaries |
Why This Team Model Works
- No Single Person Can Recover Alone → System Accountability
- No Therapist Alone Can Deliver 360° Change → Multi-Role Support
- Client is Never Left Unsupervised → Confidence + Consistency
- Every Dimension of OCD is Targeted → Permanent Recovery
In Simple Words (Client-Facing Explanation)
You are not working with one therapist. You are backed by a complete team.
A Lead OCD Specialist guides your recovery path, ERP therapist makes you practice exposures, wellness coach stabilizes your body and mind, and daily support coach makes sure you don’t slip. You are guided every single day until OCD loses power completely.
Success Stories of “Something Bad May Happen” OCD Recovery at Emotion of Life
1. “What if something terrible happens to my parents?”
Client: 22-year-old Female, Delhi
Problem: Constant fear that parents will die if she doesn’t pray repeatedly.
Symptoms:
- Repeating prayers 100+ times a day
- Seeking reassurance every 30 minutes
- Emotional breakdowns at night
Recovery Journey at Emotion of Life:
Through ERP, she practiced allowing intrusive fear without doing the prayer ritual.
She learned emotional acceptance and cognitive restructuring to break the “fear = truth” belief.
Daily accountability coaching helped her stay consistent.
Outcome:
In 5 months, she stopped compulsive prayers, sleeps peacefully, and now travels and lives independently without fear.
Her Words:
“I realized the fear was not reality. I learned to trust myself and life again.”
2. “If I leave the house, something bad will happen to my younger sister.”
Client: 28-year-old Male, Bangalore
Problem: Avoided going out because of obsessive fear that his actions could cause harm to his sister.
Symptoms:
- Cancelled office work frequently
- Kept checking on sister 20–25 times a day
- Heavy anxiety and guilt
Recovery Process:
Customized ERP exposures were designed:
- Leaving home without checking
- Not calling sister for hours
- Tolerating uncertainty and discomfort
Daily journaling + follow-up ensured stability.
Outcome:
After 4.5 months, he is regular at work, no safety checks, and guilt dissolved.
His Words:
“I learned that love doesn’t mean protection through fear. I am free.”
3. “Something bad will happen if I make the wrong choice.”
Client: 19-year-old Student, Mumbai
Problem: Fear of making decisions due to belief that wrong choice = disaster.
Symptoms:
- Decision paralysis
- Asking family for reassurance
- Constant overthinking and self-criticism
Recovery at Emotion of Life:
CBT work targeted guilt, doubt, and perfectionism.
ERP involved making small decisions without reassurance, then bigger ones.
Gradual exposure normalized uncertainty.
Outcome:
In 3 months, she began taking independent decisions confidently.
Now attending college and planning to study abroad.
Her Words:
“I am allowed to choose, grow, and learn. Fear no longer controls me.”
4. “I always felt something terrible will happen if I don’t check everything repeatedly.”
Client: 35-year-old Male, Dubai
Problem: Fear that car, gas, doors, and appliances could cause accidents.
Symptoms:
- Checking car locks 50+ times
- Repeatedly confirming gas knobs
- Late arrivals to work
Recovery Approach:
Step-by-step ERP Ladder:
- Leaving home without checking
- Reducing checking cycles gradually
- Practicing “leave and don’t return” method
Lifestyle coaching improved sleep and emotional stability.
Outcome:
After 6 months, checking behavior reduced to almost zero.
He now leaves the house calmly in under 3 minutes.
His Words:
“Peace is not the absence of risk, it’s the presence of trust.”
5. “I believed something terrible will happen to my baby because of my thoughts.”
Client: 32-year-old New Mother, Hyderabad
Problem: Postpartum Harm-OCD (fear that thoughts will cause harm to her child).
Symptoms:
- Avoided holding and bathing the baby
- Constant guilt and crying
- Fear of being a “bad mother”
Recovery at Emotion of Life:
ERP + Self-compassion work helped her separate thought from reality.
Gradual exposure to baby handling restored trust.
Wellness coaching stabilized hormonal emotional fluctuations.
Outcome:
Within 4 months, she bonded normally with her child, cares with confidence, and no longer fears her thoughts.
Her Words:
“I realized my thoughts were symptoms, not truth. I got my motherhood back.”
When to Seek Professional Help
If intrusive fears interfere with daily life, relationships, sleep, work, or decision-making, specialized OCD treatment is recommended. Early intervention leads to better long-term outcomes.
Frequently Asked Questions (FAQ)
Is “Something bad may happen” OCD curable?
OCD is highly treatable. Many individuals experience complete functional recovery with structured therapy and lifestyle intervention.
Can these thoughts become reality?
No. Intrusive thoughts are not predictions; they are mental noise generated by an overactive fear circuit.
Is this OCD the same as anxiety?
OCD involves intrusive thoughts + compulsions; anxiety is a general emotional state. They often co-occur.
Do I need medication?
Not always. Many individuals recover through structured non-pharmacological programs like ERP and holistic behavioural therapy.
Conclusion on “Something Bad May Happen” OCD
“Something bad may happen” OCD can feel terrifying, but it is one of the most well-understood and highly treatable subtypes of OCD. With the right therapeutic framework, individuals can break free from catastrophic thinking, reduce compulsions, and rebuild trust in themselves and their environment.
Structured treatment, especially non-medicine holistic programs such as the Emotion of Life model, provides a clear pathway to meaningful recovery and long-term resilience.
Contact: Email: info@emotionoflife.in
Phone/WhatsApp: 9368503416 Call for Initial Discussion
Emotion of Life — OCD Treatment, Research & Training Institute. Lead Specialists: Shyam Gupta & Pratibha Gupta. We treat 70+ OCD subtypes and specialize in complex, chronic, and treatment-resistant cases. Non-medication recovery using CBT, ERP, and holistic wellness integration.
Book Now | Review | OCD Types | Our Experts | Success Stories| Contact Us| MyPsychologist