Body Dysmorphic OCD — Symptoms, Causes & Treatment
Overview
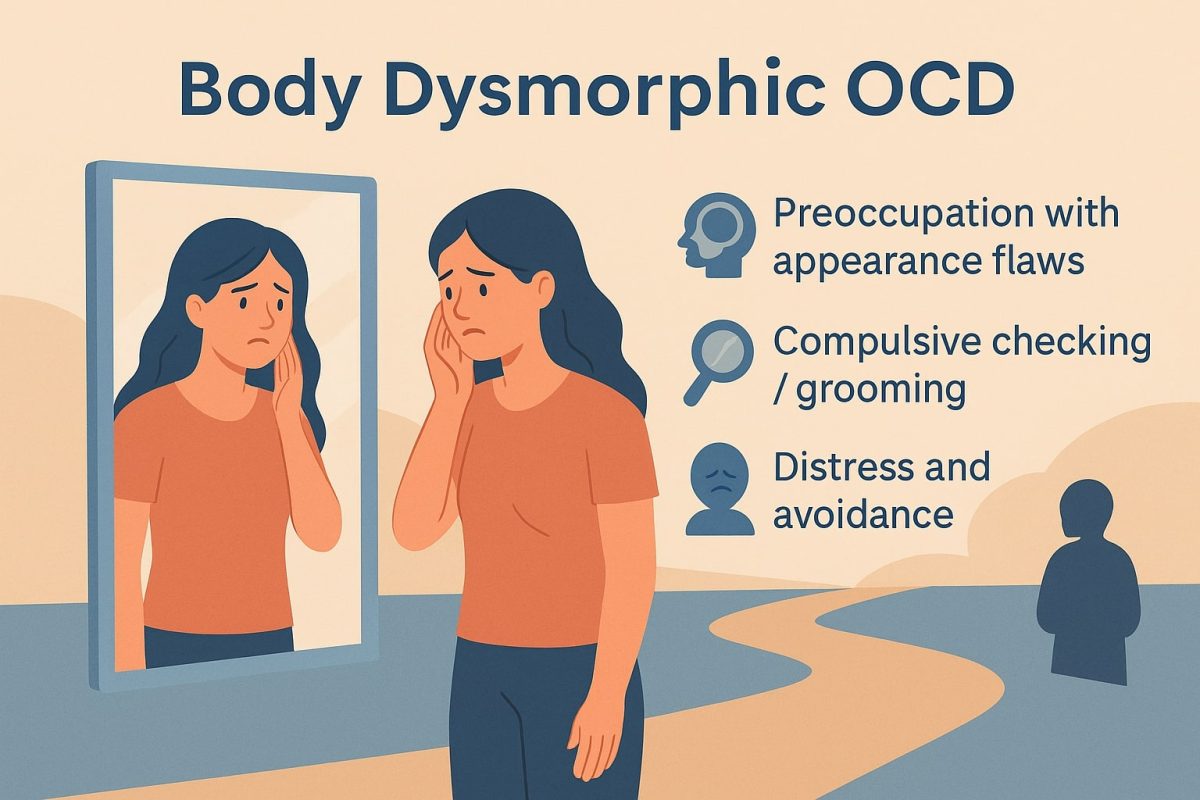
Body dysmorphic OCD is a troubling and often concealed condition characterized by obsessive thoughts focused on imagined flaws in one’s appearance. Individuals affected by body dysmorphic concerns experience intrusive thoughts about specific body parts — for example believing their nose is “too large,” their skin is “disfigured,” or their hair is “unappealing.” These thoughts commonly trigger compulsive behaviours such as mirror checking, hiding perceived flaws, seeking reassurance, or repeatedly seeking cosmetic fixes.
When obsessions and compulsions consume significant time, damage relationships, or result in repeated cosmetic procedures, the problem has moved beyond ordinary dissatisfaction into a clinical issue.
Body Dysmorphic OCD: How it relates to BDD and OCD
Body dysmorphic OCD sits at the intersection of obsessive thinking and body-image disturbance. It differs from normal concern about looks because it is persistent, intrusive, and functionally impairing. Underlying mechanisms include low tolerance for uncertainty, exaggerated error monitoring, and an overvaluation of appearance for self-worth.
In some cases, people experience perceptual distortions — genuinely seeing minor imperfections as major defects. This, combined with compulsive behaviours (mirror rituals, grooming, camouflage), fuels a self-perpetuating cycle of distress.
Symptoms of Body Dysmorphic OCD
Symptoms vary but often follow a recognizable pattern:
- Intrusive, repetitive thoughts about appearance that feel difficult to control.
- Prolonged mirror checking (often with magnification or strong light) or complete mirror avoidance.
- Camouflaging behaviours (excessive makeup, specific clothing, hair styling to hide perceived flaws).
- Frequent reassurance seeking from family, friends, or professionals.
- Compulsive comparison with others (browsing photos, comparing features).
- Emotional consequences such as shame, social withdrawal, depression, and anxiety.
Origin & Risk Factors
Psychological origins
Early experiences — teasing about appearance, strict or appearance-focused parenting, or internalized cultural messages that equate worth with looks — can prime vulnerability. Personality traits such as perfectionism, self-criticism, and intolerance of uncertainty also increase risk.
Environmental triggers
Events like puberty, acne, weight change, or heavy exposure to idealized images (social media, advertising) can trigger or worsen symptoms. Cosmetic interventions often fail to address the underlying obsession and may even reinforce it.
Treatment Options
Treatment is evidence-based and multifaceted — combining psychological therapies, lifestyle changes, and coaching/support:
Cognitive Behavioral Therapy (CBT)
CBT adapted for body-dysmorphic concerns helps clients identify and challenge distorted beliefs (e.g., “My value depends on my looks”), and use behavioural experiments to test those beliefs in real life. CBT also targets compulsive comparisons and reduces problematic social media use.
Exposure and Response Prevention (ERP)
ERP is a core behavioural approach. For body dysmorphic OCD, mirror exposure is commonly used: the person practices looking in a mirror for set periods while resisting checking or other rituals. Over time, anxiety habituates and rituals decrease. Other ERP exercises include resisting cosmetic reassurance, brief camouflage exposures, and attending social events without safety behaviours.
Acceptance and Commitment Therapy (ACT)
ACT complements CBT/ERP by teaching cognitive defusion — seeing thoughts as mental events rather than truths — and by helping individuals act in line with their values (relationships, creativity, career) despite appearance-related anxiety.
Wellness Coaching & Lifestyle Work
Wellness coaching strengthens recovery by improving sleep, routine, nutrition, exercise, and reducing triggers (like social media). Coaches help clients build sustainable habits that reduce the “fuel” for dysmorphic thinking.
Personality Dynamics & Long-Term Work
Therapy that addresses perfectionism, shame, and self-criticism helps rewrite old messages (e.g., “You must always look perfect”) and replace them with compassionate, resilient self-beliefs.
Practical Coping Strategies
- Grounding and brief mindfulness to reduce physiological arousal.
- Scheduled “mirror time” to limit checking.
- Choosing a single trusted person for reality checks instead of multiple reassurance requests.
- Thought records, visual reality testing, and self-compassion scripts.
Improving Emotional & Social Health
Body dysmorphic OCD often coexists with depression and social anxiety. Family therapy can educate loved ones about unintentional reinforcement (reassurance, enabling). Peer support and group therapy can reduce shame and isolation. Emotional regulation work — creativity, volunteering, meaningful roles — helps restore self-worth beyond appearance.
Success Stories
Success Story I — Ankit (28)
Ankit, a graphic designer, spent years scrutinising his skin for an hour each morning. After CBT + ERP + ACT and wellness coaching at Emotion of Life, his checking rituals reduced, he resumed photography, and he now describes recovery as learning to live freely rather than becoming “perfect.”
Success Story II — Reema (25)
Reema developed a fixation on her nose after a classmate’s comment. Through focused CBT, ERP, and personality work she gradually stopped camouflaging, rejoined internships and social life, and rebuilt confidence based on values and action rather than reflection.
FAQ
1. How is Body Dysmorphic OCD different from normal body insecurity?
Normal insecurity is occasional and non-disruptive. Body dysmorphic OCD involves intrusive, repetitive thoughts and behaviours that significantly interfere with daily functioning and relationships.
2. What are common symptoms?
Mirror checking, excessive grooming, camouflaging, avoidance of social situations, comparison behaviour, and reassurance seeking — accompanied by shame, anxiety, or depression.
3. What causes Body Dysmorphic OCD?
Causes are multi-factorial: psychological traits (perfectionism), early experiences (teasing), and environmental exposure (social media, life events) all contribute.
4. Can lifestyle changes or wellness coaching help?
Yes — lifestyle changes and coaching support therapy by stabilising routine, reducing triggers, and providing structure for recovery.
5. Can Body Dysmorphic OCD fully remit?
Many people achieve significant improvement or long-term remission with consistent therapy, ERP, ACT, and lifestyle support. Intrusive thoughts may reappear occasionally but become less powerful and less disruptive.
Conclusion
Body dysmorphic OCD is a painful convergence of obsessive thinking and appearance concerns, but it is treatable. A compassionate, evidence-based blend of CBT, ERP, ACT, wellness coaching, and deeper personality work helps people reclaim time, relationships, and purpose. Recovery emphasises living a meaningful life rather than attaining a flawless appearance.
Seek Help — Emotion of Life
If you or someone you care about is struggling with appearance-focused obsessions, seeking specialised support is a courageous step.
Call: +91 93685 03416
Website: www.emotionoflife.in
Email: info@emotionoflife.in
Book Now | Review | OCD Types | Our Experts | Success Stories| Contact Us| MyPsychologist