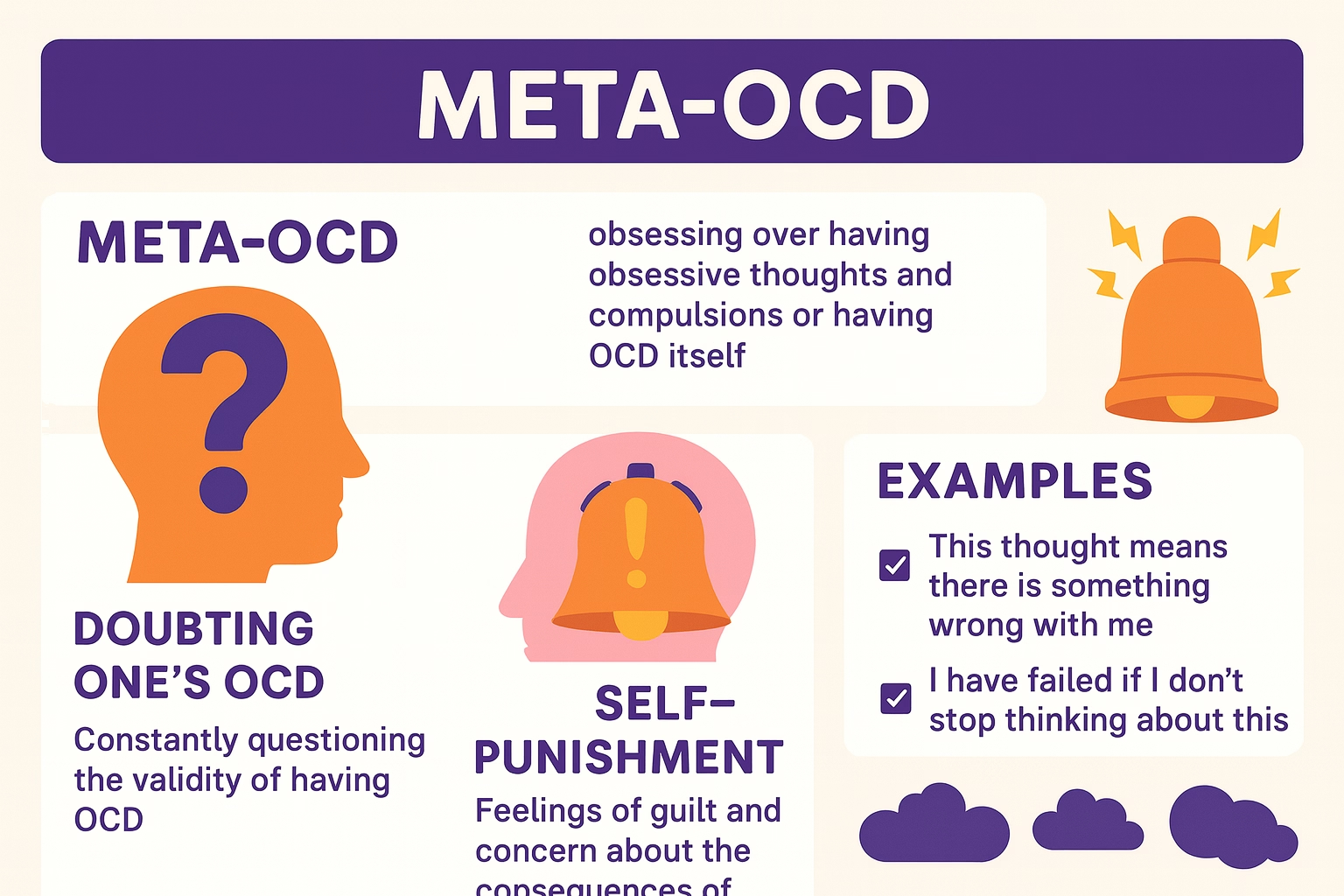
Meta OCD often called OCD of OCD, is a pattern where a person becomes obsessively preoccupied with the possibility of having OCD, the correctness of the diagnosis, or whether their thoughts are “really OCD” versus something worse. Instead of focusing on contamination, symmetry, or harm themes, the obsession targets OCD itself turning the mind into a constant diagnostic scanner.
This is different from normal self-reflection. In Meta OCD, doubt and fear spiral: “Do I have OCD? What if I’m just faking it? What if I’m beyond help?” These questions don’t resolve with logic. They act like quicksand— in Meta OCD the more you struggle to prove certainty, the deeper you sink. The result is a cycle of checking, reassurance-seeking, self-monitoring, and compulsive research, which ironically strengthens OCD.
Good news: Meta OCD responds very well to structured, skills-based treatment. At Emotion of Life in India, we help clients recover—often without medication—using CBT (Cognitive Behaviour Therapy) and ERP (Exposure and Response Prevention), and focusing on wellness aspect and upgrading principle of life, doing course correction in personality dynamics which are reason of developing and maintaining OCD in Human life. With unique model of care as OCD Recovery and Cure Program with 16 steps of OCD Recovery Process guided by Shyam Gupta OCD Specialist Therapist & Rehabilitation Psychologist and Pratibha Gupta Female OCD Therapist and wellness coach Mrs. Aisha.
How Meta OCD Differs from General OCD
- Theme focus:
- General OCD themes: contamination, harm, sexual/relationship, religious/scrupulosity, symmetry/ordering, health, etc.
- Meta OCD: the status of having OCD itself diagnosis doubt, treatment doubt, fear of mislabeling, fear of “not having real OCD,” or anxiety that one will never recover.
- Compulsions shift inward:
in Meta OCD Instead of washing or arranging, compulsions are primarily cognitive: mental checking (“does this feel like OCD?”), rumination, reassurance-seeking about the diagnosis, reading endless articles, switching therapists, and comparing symptoms. - Goal distortion:
The hidden compulsion in Meta OCD is to achieve absolute certainty: perfect diagnosis, perfect treatment steps, perfect proof of being “really OCD.” In evidence-based care, we aim for tolerance of uncertainty, not perfect certainty. - Misleading sense of insight:
People with Meta OCD often sound insightful because they can articulate the OCD model yet they remain trapped by compulsions done in the name of clarity. Insight without response prevention becomes another ritual.
Why Meta OCD Creates a Self-Doubt Loop
- Intrusive doubt pops up: “Maybe I’ve misdiagnosed myself.”
- Anxiety spikes → discomfort feels urgent.
- Compulsive response to feel sure: Googling, asking therapists/friends, reading forums, mentally checking how the thought “feels.”
- Anxiety reduces temporarily → the brain learns that reassurance equals relief.
- Next doubt returns, stronger and broader → the cycle tightens.
In Meta OCD is classic negative reinforcement: the short-term relief from compulsions keeps OCD alive. The exit door is CBT process with ERP reducing compulsions and building tolerance for not knowing with 100% certainty. Ironically, certainty grows naturally as you stop feeding the loop.
Signs and Symptoms of Meta OCD
- Obsessional themes in Meta OCD
- Persistent worry about whether you truly have OCD
- Fixation on whether specific thoughts “count” as intrusive or bad
- Fear that you’re faking symptoms or doing therapy “wrong”
- Doubts about whether recovery is possible for “someone like me”
- Hyper-monitoring internal states in Meta OCD: “Did that thought feel like OCD or real me?”
- Common compulsions in Meta OCD
- Mental rituals: replaying conversations, analyzing past feelings, internally debating diagnosis
- Reassurance-seeking: repeatedly asking loved ones or therapists, “Is this OCD? Will I be okay?”
- Research binges in: reading articles/videos for hours, hopping between therapists or programs
- Self-tests: creating rules like “If I think X tomorrow morning, then it’s OCD; otherwise it’s not”
- Avoidance in: avoiding therapy sessions, difficult topics, or triggers that produce diagnostic doubt
- Functional impact of Meta OCD
- Reduced productivity due to rumination
- Emotional exhaustion; sleep disruption
- Delayed or derailed treatment progress
- Strained relationships from frequent reassurance cycles
Common Thought Patterns in Meta OCD
- All-or-nothing certainty: “If I can’t be 100% sure it’s OCD, I shouldn’t proceed.”
- Catastrophizing: “If this isn’t OCD, then my life is ruined.”
- Intolerance of uncertainty: “Not knowing is unbearable.”
- Mental filtering: Fixating on exceptions “That one time it felt different, so this can’t be OCD.”
- Reassurance addiction: Treating certainty as a relief drug rather than a skill to practice less of.
CBT helps label these patterns and replace them with flexible, reality-tested thinking.
Psychological Causes and Maintaining Factors of Meta OCD
- Baseline anxiety + intolerance of uncertainty: A temperament that craves clarity under stress.
- Perfectionism: The urge to “diagnose perfectly,” “do therapy perfectly,” or “recover perfectly.”
- Hyper-responsibility: Belief that mislabeling a thought could have dire consequences.
- Reassurance conditioning: Past experiences where reassurance brought relief, reinforcing the cycle.
- Information overload: in Meta OCD constant online content can become a compulsion arena instead of education.
Meta OCD vs Health Anxiety & Reassurance-Seeking
Meta OCD overlaps with health anxiety in structure: intrusive alarm → body/mind scanning → checking → temporary relief. Instead of physical symptoms, Meta OCD scans mental experiences (feelings, thoughts, urges). Both heavily rely on reassurance, which becomes the fuel of the disorder.
Recovery in both conditions involves exposure to uncertainty and limiting reassurance. In Meta OCD, we practice living with imperfect diagnostic certainty and accepting fluctuations in how “OCD-ish” something feels on a given day.
How Diagnosis and Misdiagnosis Play In OCD of OCD
It’s wise to get a professional assessment, ideally from an OCD specialist. However, once a credible evaluation supports OCD, chasing second-to-hundredth opinions becomes another ritual. The therapeutic stance is:
“We have enough information to begin evidence-based treatment, even if my brain still wants 100%.”
Treatment that Works: CBT + ERP (Without Medication)
At Emotion of Life, we specialize in non-medication recovery pathways using structured CBT and ERP, personalized coaching, and daily practice plans. As medication can not be helpful for most of people in Meta OCD. many clients recover without it through methodical skill building.
Core CBT Skills for Meta OCD
- Psychoeducation: Understand how reassurance and rumination wire OCD.
- Cognitive restructuring (used carefully): Identify thinking traps (catastrophizing, all-or-nothing). We don’t argue endlessly with thoughts; we acknowledge them and choose values-based action.
- Uncertainty practice: Create small daily exercises to allow not knowing (e.g., “Maybe it’s OCD, maybe it’s not; I’m still living my day”).
- Behavioral activation: Re-enter life domains OCD stole—work, relationships, hobbies—without completing mental checks first.
ERP: Exposure and Response Prevention
- Exposure: Gently and intentionally bring on the doubt trigger (e.g., reading an article about OCD without trying to “confirm” your case).
- Response prevention: Do not perform the usual rituals (no Googling, no reassurance questions, no mental debates).
- Learning goal: Teach the brain that anxiety can rise and fall on its own, and you can function without certainty rituals.
Practical ERP Examples for OCD of OCD
Note: Always tailor with a specialist. Start small and build.
- Planned uncertainty statements
- Exposure: Read a card 3–5 times daily “Maybe I have OCD, maybe I don’t.”
- Response prevention: Resist internal debates that try to resolve the “maybe.” With logic and rationality required in life.
- Learning: You can carry uncertainty and still live your values.
- Limit reassurance experiments
- Exposure: Go 48 hours without asking anyone if your symptoms are “really OCD.”
- Response prevention: If the urge hits, jot it in a log and ride the wave.
- Learning: Urges peak and fall reassurance isn’t required.
- Article exposure without checking
- Exposure: Read 1–2 reputable OCD resources.
- Response prevention: No symptom-matching, no self-tests, no extra Googling.
- Learning: Information can be taken in without compulsive comparison.
- Trigger scripts (imaginal exposure)
- Example script: “What if I don’t have OCD and I’m wasting time? Then I’ll have practiced uncertainty skills that help all humans. Life will still move forward.”
- Response prevention: Sit with discomfort; don’t chase a perfect rebuttal.
- Delay & diminish ritual
- Exposure: When the urge to Google arises, set a 20-minute timer.
- Response prevention: During the delay, do a valued action (email, walk, task).
- Learning: Urges often fade or become manageable.
Mindfulness-Based Strategies That Support ERP
- Label, don’t analyze: “Noted: diagnostic doubt.” Move attention to a task.
- Breath + anchor: 3 slow breaths, feel feet on the ground; continue your activity.
- Willingness mantra: “I allow uncertainty to be here while I live my values.”
- Attention shifts: Schedule two 10-minute windows for journaling doubts; outside those windows, redirect. This prevents all-day rumination.
Recovery Routines You Can Start Today
- Daily uncertainty reps (2–5 minutes): Read your flexibility statements; notice urges; resist rituals.
- Reassurance: do reassurance once with your therapist only.
- Compulsion tracking: Use a simple tally in your phone. The goal isn’t zero instantly it’s steady reduction.
- Values calendar: Schedule meaningful, practical activities first (workout, call a friend, a project block). OCD rides with you; it doesn’t drive.
- Sleep and basics: Regular sleep, movement, and nutrition stabilize reactivity.
- Therapy consistency: Stick to one program long enough to see learning not day-to-day switching.
Family & Partner Guidance
- Replace reassurance with validation: “I know this feels hard. I’m confident you can use your skills.”
- Use a family plan: When asked, reply with an agreed sentence (e.g., “I won’t give reassurance, but I’ll sit with you while it passes”).
- Celebrate skill use, not anxiety reduction: “I’m proud you rode that wave,” rather than “I’m glad you feel better now.”
Real-Life Success Story Meta OCD (Non-Medication) from Emotion of Life
Riya 26, arrived at Emotion of Life exhausted. She’d spent months reading about OCD, booking consultations, and changing therapists whenever doubt resurfaced: “What if I don’t actually have OCD? What if I’m just making excuses?” She asked her partner for reassurance multiple times a day and tracked “OCD feelings” in an app, hoping to hit a perfect pattern that proved the diagnosis.
Under Shyam Gupta’s guidance, we created a 20-week daily CBT + ERP plan focused on Meta OCD:
- Week 1–2: Psychoeducation on the reassurance loop; building a Reassurance Reduction Agreement with her partner.
- Week 3–4: Uncertainty statements and delay rituals; beginning article exposures without checking.
- Week 5–6: Imaginal scripts around her worst-case fear (“What if I’m misdiagnosed and waste time?”).
- Week 7–9: Values activation—return to a paused design course, social plans, minimal symptom-checking.
- Week 10–12: Consolidation—tougher triggers (podcasts, forums) without comparison rituals.
- Week 13 to 20: Relapse management triggering client in control environment and follow up and other need like skills building and practices.
By Week 6, reassurance dropped from 15 times/day to 3/day. By Week 10, she reported going 72 hours without any reassurance and finishing two course modules she’d delayed for a year. At completing journey, she described herself as “functioning freely with uncertainty,” sleeping better, and living more than analyzing. She chose to stay off medication, crediting structured ERP and daily coaching with her recovery.
Note: Every client is unique. Most clients recover fully without medication; some choose combined approaches which is not recommended in Emotion of Life as its slow down OCD recovery process. The unifying factor is consistent ERP and values-based action.
Frequently Asked Questions (FAQ)
Q1: How do I know if this is Meta OCD and not a real diagnostic concern?
Get an evaluation from an OCD-trained professional. If OCD is reasonably supported, treat the urge for perfect certainty as part of the disorder. Proceed with CBT + ERP while practicing uncertainty tolerance.
Q2: Won’t ignoring my doubts make things worse?
We don’t ignore—we observe and allow without performing compulsions. ERP teaches your nervous system that you can handle doubt, reducing its power.
Q3: Can I recover without medication?
Many do, through structured CBT + ERP, mindfulness, and lifestyle supports. We design non-medication pathways at Emotion of Life; decisions are always individualized.
Q4: What if my doubt feels different every day?
Meta OCD often morphs. ERP targets the process (doubt → compulsion), not every content variation. Skills generalize as themes shift.
Q5: How long does recovery take?
Timelines vary. What matters is consistency: small daily exposures, relentless response prevention, and values-based living. Usually 5 months daily session is enough for complete recovery from Meta OCD.
When to Seek Professional Help
- Your day is dominated by rumination and reassurance-seeking
- Work, study, or relationships are suffering
- You start to avoid therapy or triggers to keep doubt away
- You’ve tried “self-help by research” for months without progress
Specialized support accelerates recovery by providing safety, structure, and accountability.
Why Choose Emotion of Life for Meta OCD
- Expertise in OCD only: We focus deeply on OCD subtypes, including Meta OCD.
- Structured non-medication pathways: CBT + ERP, mindfulness, and wellness coaching.
- Daily practice plans & coaching: Implementation support between sessions.
- Online and onsite (Agra) options: Flexible access for clients across India and abroad.
- Led by Shyam Gupta: OCD Specialist Therapist & Rehabilitation Psychologist with decades of experience of 24 years in guiding and transforming OCD clients from OCD bettel to OCD recover and cure state that is also without medication.
A Sample One-Week Meta OCD Practice Plan
Day 1–2:
- Read uncertainty card (3×/day): “Maybe this is OCD, maybe it isn’t. I choose values anyway.”
- Delay Googling by 20 minutes; do a valued task in the gap.
Day 3–4:
- Article exposure: read one OCD article without symptom-matching.
- Log reassurance urges; respond with the family plan script.
Day 5–6:
- Imaginal script: “What if I’m misdiagnosed?” Listen/read for 10 minutes; no rebuttal.
- Re-enter one avoided activity (study block, gym visit, social call).
Day 7:
- Review wins: count skills used, not hours felt good.
- Plan next week’s “+10% difficulty” exposure.
(Always tailor with a professional; start where it’s safe and workable.)
Key Takeaways
- Meta OCD is OCD focused on OCD itself—obsessing about diagnosis, certainty, and doing therapy “right.”
- The core trap is reassurance-seeking and mental checking; the cure is tolerating uncertainty.
- CBT + ERP are gold-standard treatments; many people recover without medication with structured practice.
- A consistent, values-oriented plan—like those offered by Emotion of Life under Shyam Gupta’s guidance—restores freedom.
Conclusion: OCD Cure Is Possible with Structured Therapy
“OCD of OCD” feels paradoxical—like the mind is stuck in a hall of mirrors, checking whether it’s checking correctly. Yet the pathway out is refreshingly practical: face doubt on purpose, reduce reassurance, and live your values now. With CBT + ERP, supportive coaching, and a steady routine, your brain learns a new truth: certainty isn’t required to live fully.
At Emotion of Life, we have seen clients reclaim careers, relationships, creativity, and calm—without medication—by committing to the process. If Meta OCD has been running your days, remember: you don’t need perfect certainty to begin. Start with one small exposure, prevent one ritual, and keep going. Recovery isn’t a riddle to solve; it’s a skill you practice—and it works.
Ready to Start?
If you’d like a personalized CBT + ERP plan for Meta OCD (online or onsite in Agra), we’ll help you design daily practices, coach you through exposures, and support non-medication recovery—guided by Shyam Gupta at Emotion of Life.